- Search
| Ann Coloproctol > Volume 38(3); 2022 > Article |
|
Abstract
Purpose
Anastomotic leakage, a known major postoperative complication, potentially leads to readmission, reoperation, and increased mortality rates in patients, such as rectal cancer patients following a low anterior resection (LAR). Currently, vacuum-assisted closure, as featured by B-Braun (B-Braun Medical B.V.), is already being used for the treatment of gastrointestinal leakages and fistulas. The main aim of this study was to introduce a novel method for creating a vacuum-assisted drain for the treatment of anastomotic leakage after LAR.
Methods
All 10 patients, who underwent LAR surgery from 2018 to 2019, were diagnosed with anastomotic leakage and had received neoadjuvant chemotherapy prior to surgery. Therefore, patients were treated with a handmade vacuum-assisted drain and were revisited every 5 to 7 days for further evaluations and drain replacement until leakage resolution. Physical features of cavity, time of diagnose, and duration of treatment were analyzed correspondingly. The handmade vacuum-assisted sponge drain was prepared for each patient in each session of follow-up.
Results
Eight out of 10 patients experienced complete closure of the defect. The mean delay time from the day of operation to the diagnosis of anastomotic leakage was 61.0┬▒80.4 days while the mean time for leakage closure was 117.6┬▒68.3 days. Eventually, 7 cases underwent ileostomy reversal with no complications during a 3-month follow-up.
Anastomotic leakage is one of the major complications following colorectal surgeries. It often requires further reinterventions and hospitalization, which may lead to higher rates of morbidity and mortality. Low anterior resection (LAR) is the standard operation for upper- and mid-rectal cancers. The incidence of leakage in this operation has been reported up to 36% with a mortality of 6% to 22% [1]. Vacuum-assisted closure (VAC) has been used for gastrointestinal leakages and fistulas [2-4], thus, allowing sepsis control and facilitation of the healing process. Endo-SPONGE (B. Braun Medical B.V., Melsungen, Germany) is a commercially available sponge VAC tool designed and used for postoperative rectal anastomotic leakages [5, 6]. Even though it is a useful tool as a negative pressure vacuum therapy, the cost of the device can be a problem since it may need to be replaced a number of times for the treatment of 1 patient. For this reason, we have designed a simple handmade VAC device with similar effects that can easily be made with tools and materials available in a general surgery operating room. Overall, we treated 10 patients with complicated anastomotic sinus cavities following LAR surgery using these handmade devices. In this article, we will illustrate the steps used for making this handmade vacuum-assisted sponge drain as well as the outcome of the patients using these devices following LAR surgery.
In this study, a total of 10 patients, which were diagnosed with an anastomotic leakage or defect in the anastomotic line following LAR surgery due to rectal cancer, were included prospectively from 2018 to 2019. All patients were experiencing rectal cancer located in the mid or lower rectum. After primary resection, all of the anastomosis were located in the lower third of rectum (less than 6 cm from the anal verge). One of the cases was in stage 2 (T3N0M0) and 8 patients were in stage 3. One case was in stage 4 (T4N2M1) who had a previous liver metastasectomy before. All patients had received neoadjuvant chemoradiotherapy before the primary operation. All of the cases underwent LAR surgery and diverting ileostomy placement in the same operation. Three patients had a history of type 2 diabetes mellitus treated with oral agents. Moreover, an end-to-end anastomosis was performed using a 28- or 32-mm circular stapler. All of the patients experienced routine rectosigmoidoscopy 30 days after surgery and then every 3 months for 1 year. Also, any sign of local leaks such as perineal pain or pus discharge from the anus indicated doing rectosigmoidoscopy and computed tomography scan with intravenous and rectal contrast for the patient. Any sign of anastomosis defect was considered as leakage and the patient was included in this study (Fig. 1).
Patients experiencing complete anastomotic failure, signs of severe sepsis, tumor recurrence at the anastomotic site, or patients clinically inappropriate for multiple operations were excluded from this study. Informed consent was obtained from all the patients. This study was approved by the Ethical Committee of Imam Khomeini Hospital Complex (No. IR.TUMS.IKHC.REC. 1399.303) affiliated by Tehran University Of Medical Sciences.
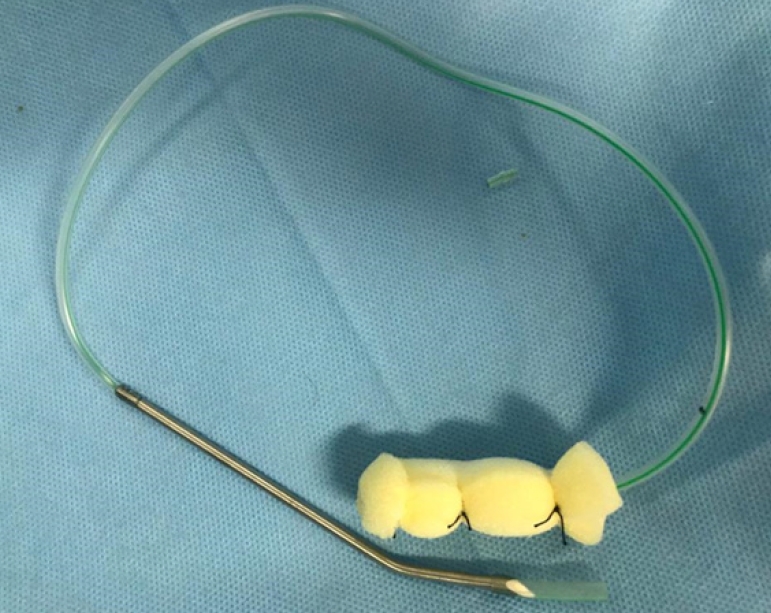
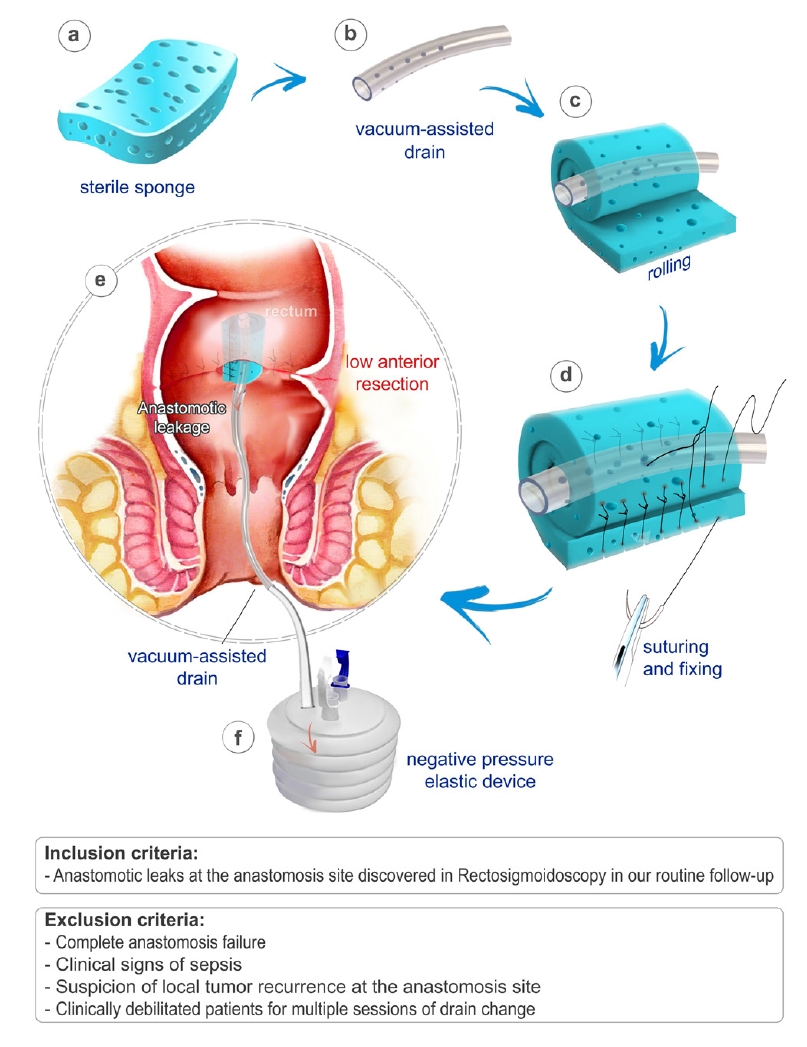
To make a vacuum-assisted sponge drain for anorectal anastomotic defects, we used an open-pored polyurethane sponge (Vaccare, Tehran, Iran), a tube drain connected to a negative pressure elastic device named Hemovac (e.g., Redivac drain, Supa Medical Devices, Tehran, Iran), and a 0 braided silk suture (Supa Medical Devices).
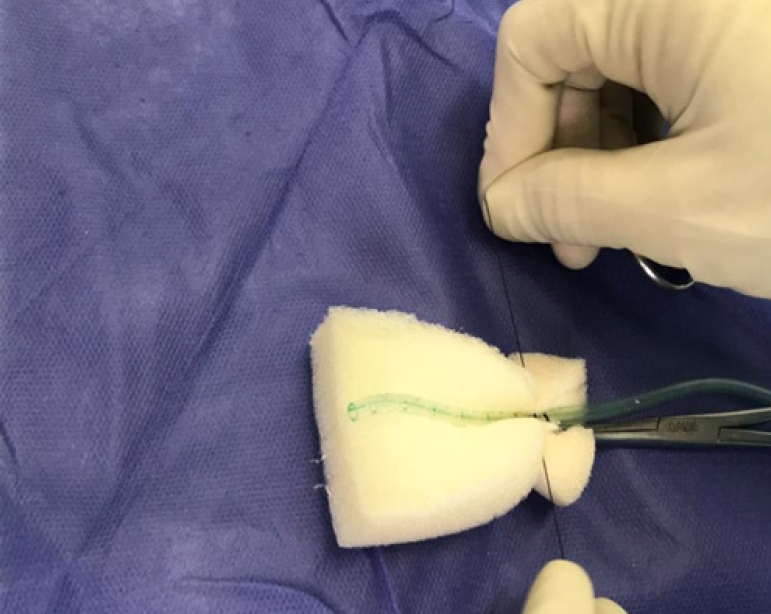
General or spinal anesthesia was not needed since the whole procedure takes 10 to 15 minutes. Under intravenous sedation and in the lithotomy position the anal canal is examined followed by the rectum using an anal self-retractor (such as a lone-star) to locate the defectŌĆÖs site; if there is any collection, it requires suctioning to ensure that the tract is clean. Furthermore, irrigation with saline may be necessary. The size of the cavity should be estimated by digital examination or by the use of a measuring tool. The sponge is trimmed to the formerly assessed size of the cavity. Next, the sponge is wrapped around the tip of the drain. By using a silk suture, the sponge is fixed around the drain in at least 2 or 3 separate locations. Make sure to move the needle across the holes of the drain to prevent its separation. Then circle it around the sponge and tie it firmly (Figs. 2, 3). To introduce the sponge into the cavity, grasp the end of the sponge and drain with a long clamp or ring forceps inserting it gently into the cavity. Release the clamp and use it to push the sponge further into the cavity. Care must be taken to avoid any direct contact between the drain and the mucosa. The drain is then taped to the lateral side of 1 of the buttocks. There is no need to fix or suture the tube to the skin, as it will cause severe pain for the patient.
After surgery, no activity restriction was advised. However, we recommended patients avoid drain manipulation. The patients were admitted to the operation room every 5 to 7 days and the drain was replaced with the same method every session. It should be emphasized not to leave the sponges in their place for more than a week because the adhesion of the sponge to the surrounding tissue could make the sponge removal difficult. This process was continued until the defect of the internal orifice was smaller than 1 cm. The cavity size was estimated by inserting a suction into the cavity, hence, measuring its length into the cavity. Subsequently, it was left to be closed by itself and the patients were followed up by monthly rectoscopies. The evaluated features of leakage are noted in Table 1. Without being limited to a specific duration of treatment, successful treatment was defined as a complete closure of the cavity as observed in the flexible rectoscopy examinations. In addition, cavity enlargement or the development of signs of sepsis were considered indications for the termination of this treatment. A graphical abstract is illustrating the steps above (Fig. 1).
In this study, 10 patients were treated between August 2018 to June 2019, including 6 males and 4 females with a mean age of 55.8 ┬▒ 10.8 years (mean ┬▒ standard deviation). The mean delay time from the day of operation to the diagnosis of anastomotic leakage was 61.0┬▒ 80.4 days. The mean depth of the cavity was 3.75┬▒ 1.85 cm and the mean percentage of the circumferential defect was 38.0%┬▒ 19.8%. Furthermore, the mean time for leakage closure was 117.6┬▒ 68.3 days. All of our patients had received neoadjuvant chemotherapy prior to surgery. In addition, the anastomoses were located within the lower rectum (less than 8 cm from the anal verge), which was easily accessible transanally in all of the patients. Demographic and clinical features of patients are shown in Table 1. Eight cases were successfully treated using the sponge drains, which means the cavity was resolved completely in rectosigmoidoscopy examination. Nonetheless, anastomotic failure occurred in only 2 of the cases, ultimately leading to reoperation and permanent end colostomy placement.
In summary, out of the 10 patients, 5 cases were treated without complication and underwent a stoma reversal immediately after treatment (50.0%). Moreover, 2 cases faced anastomotic disruption (20.0%) and underwent permanent colostomy. One patient who was in stage 4 and had prior liver metastatectomy experienced liver metastasis recurrence. Although the rectal leakage was treated, the patient couldnŌĆÖt undergo ostomy reversal and was referred for chemotherapy (10.0%). Nevertheless, 3 cases had anastomotic stenosis after treatment, which were ultimately managed by dilatation. Two of these cases completely responded to dilatation and 1 experienced partial enhancement. Eventually, we did a contrast study from the distal limb of ileostomy and none of them showed signs of obstruction. So we reversed the ileostomy in all 3 cases (30.0%). No complication was observed within the 3-month follow-up in any of these cases.
Anastomotic leakage in rectal cancer is a major challenge in colorectal surgery and is associated with a high mortality rate and worse outcome [7-9]. Different causes can be proposed for the anastomotic leakage, including tension at the anastomotic site, prior radiotherapy of the rectum, and compromised vascular supply after total mesorectal excision. The leakage may cause sepsis and peritonitis, or chronic presacral sinus formations. Previously, in our institution, if the leaks did not resolve by themselves, we would go for permanent end colostomy without any other alternatives. Elsewhere, different kinds of interventions are used for the management of anastomotic leakage and its complications. VAC is a popular method for the treatment of anastomotic leakage [4, 10]. VAC is used for 2 purposes. The first purpose is to clean the cavity and drain the abscess, thus, preparing it for surgical reclosure of the anastomotic defect. The second purpose is to create negative pressure, accelerating granulation tissue formation and facilitating the closure of the anastomosis by secondary healing [11].
Due to the price of the product as well as the notion that it necessitates repeated replacement, Endo-SPONGE can become a costly treatment. Without considering the collateral costs and repeated replacements, the price of 1 set of Endo-SPONGE is 195Ōé¼ [11], while our proposed handmade device approximately costs 5Ōé¼ with a total sum of 90Ōé¼ for each session. Conversely, the use of a B-Braun VAC costs approximately 250Ōé¼ for each session. Aside from the expenses, performing a colonoscopy is needed prior to the sponge placement. Since almost all of our anastomotic leakages occurred in the low rectum, they were easily accessible by a retractor or speculum; thus, we were able to clean the cavity and place the sponge under direct vision.
We repeated the sponge replacement until the internal opening in the rectum became less than 1 cm. Then the anastomotic defect was left to be spontaneously closed within the following weeks. Although all our patients had diverting ileostomy, the necessity of ileostomy diversion in the duration of treatment is under question by previous studies [12, 13], due to the fact that the sponge fills the cavity, and prevents fecal material from reaching the sinuses. Taking into consideration all the challenges of defecation while having a rectal drain and the risk of sponge emergence, we placed a diverting ostomy for all the patients. The protective ostomy was kept open until the anastomotic sinus was completely healed. Another important fact to consider is the mechanism of anastomosis closure. Bemelman [14] proposed that by using negative pressure and drainage of the infection, new tissue is not only formed within the cavity but the neorectum also expands to fill the sinus space. However, this was different from our observation, which demonstrated that even the large sinuses were healed with time. In addition, visible granulation tissue was formed in the cavity, which was clearly distinct from the anastomosis ends. For that reason, we believe tissue expansion of the rectum as well as new tissue formation both contributes to the healing process.
Early detection of the anastomotic leakage and initiation of the VAC treatment was important throughout the treatment process. Even though our results demonstrated that early treatment had no significant effect on the duration of treatment, similar studies have supported the idea that early initiation of VAC therapy prevents further complications and failure [6, 13]. The best interval for sponge replacement is every 5 to 7 days so that enough granulation tissue is formed to prevent a challenging sponge removal. To replace the sponge more easily, irrigation of the sponge with saline is recommended before removal. Due to the size of the former Endo-SPONGE, van Koperen et al. [15] suggested earlier sponge removal (every 2 to 3 days) to prevent tissue overgrowth and ensure a less painful Endo-SPONGE removal procedure.
The long-term success of VAC treatment is unclear. Riss et al. [13] have studied 20 cases of successfully treated rectal cancer with Endo-SPONGE with a median follow-up of 17 months. They observed 5 cases of recurrent abscesses and 1 case of benign stricture. They proposed that the superficial healing of the defect along with the untreated deeper cavity might possibly be the cause of recurrence. In our experience, we observed that the depth of the sinus caused by leakage was a more important factor than the circumference of the defect. The complication of deep cavities can be overcome by the dilatation of the sinus opening as well as the continuation of sponge treatment. Deeper cavities necessitate more sessions of sponge treatment for closure. There is also a greater risk of anastomosis stricture after the treatment of large cavities; therefore, we suggest repeated colonoscopies to detect and treat stenosis in the early phases. There is also a greater risk of anastomosis stricture after the treatment of large cavities. Therefore, we suggest repeated colonoscopies to detect and treat stenosis in the early phases.
Overall, it is still unclear whether to use VAC for all anastomotic leakages since a number of cases resolve unaided without any further interventions. Nevertheless, the progression of anastomotic leakage could lead to total anastomotic disruption, resulting in a higher rate of mortality and morbidity. In consequence, we currently recommend drain placement in the sites of anastomotic leakage with the purpose of preventing unfortunate incidents.
In this study, we have introduced an innovative cost-benefit method, which can easily be prepared in the operating room. Although we evaluated the correlation between a variety of patientsŌĆÖ features and responsiveness to this method, future trials are necessary in order to achieve a more reliable conclusion.
Fig.┬Ā1.
Design and fabricate a handmade vacuum-assisted closure (VAC) for rectal anastomosis. Briefly, the sponge is trimmed to the size of the cavity (a, b) and is rolled around the drain tip while completely covers the drain (c), and is sutured to the sponge, including both parts to prevent drain removal (d). In lithotomy position, the VAC is placed in the anastomosis leakage site using a ring forceps or long clamp (e) and is connected to a negative pressure vacuum system (f).
Table┬Ā1.
Clinical and demographic features, follow-up, and outcomes of patients
REFERENCES
1. Buchs NC, Gervaz P, Secic M, Bucher P, Mugnier-Konrad B, Morel P. Incidence, consequences, and risk factors for anastomotic dehiscence after colorectal surgery: a prospective monocentric study. Int J Colorectal Dis 2008;23:265ŌĆō70.


2. Pepe G, Magalini S, Callari C, Persiani R, Lodoli C, Gui D. Vacuum assisted closure (VAC) therapyTM as a swiss knife multi-tool for enteric fistula closure: tips and tricks: a pilot study. Eur Rev Med Pharmacol Sci 2014;18:2527ŌĆō32.

3. Loske G, Schorsch T, M├╝ller C. Endoscopic intracavitary vacuum sponge therapy of anastomotic leakage in the proximal colon after right-sided colectomy. Endoscopy 2010;42 Suppl 2:E171ŌĆō2.


4. Li C, Zhao Y, Han Z, Zhou Y. Anastomotic leaks following gastrointestinal surgery: updates on diagnosis and interventions. Int J Clin Exp Med 2016;9:7031ŌĆō40.
5. Mussetto A, Arena R, Buzzi A, Fuccio L, Dari S, Brancaccio ML, et al. Long-term efficacy of vacuum-assisted therapy (EndoSPONGE┬«) in large anastomotic leakages following anterior rectal resection. Ann Gastroenterol 2017;30:649ŌĆō53.



6. Martinotti M, Ranieri V, Iiritano E, Staiano T, Dusi R, Laterza E, et al. Combined endoscopic transanal vacuum-assisted rectal drainage: a novel therapy for colorectal anastomotic leak after TME for cancer. Surg Sci 2014;5:467ŌĆō70.


7. Walker KG, Bell SW, Rickard MJ, Mehanna D, Dent OF, Chapuis PH, et al. Anastomotic leakage is predictive of diminished survival after potentially curative resection for colorectal cancer. Ann Surg 2004;240:255ŌĆō9.



8. Law WL, Choi HK, Lee YM, Ho JW, Seto CL. Anastomotic leakage is associated with poor long-term outcome in patients after curative colorectal resection for malignancy. J Gastrointest Surg 2007;11:8ŌĆō15.


9. McArdle CS, McMillan DC, Hole DJ. Impact of anastomotic leakage on long-term survival of patients undergoing curative resection for colorectal cancer. Br J Surg 2005;92:1150ŌĆō4.


10. Rosenberger LH, Shada A, Ritter LA, Mauro DM, Mentrikoski MJ, Feldman SH, et al. Delayed endoluminal vacuum therapy for rectal anastomotic leaks after rectal resection in a swine model: a new treatment option. Clin Transl Sci 2014;7:121ŌĆō6.



11. Borstlap WA, Musters GD, Stassen LP, van Westreenen HL, Hess D, van Dieren S, et al. Vacuum-assisted early transanal closure of leaking low colorectal anastomoses: the CLEAN study. Surg Endosc 2018;32:315ŌĆō27.



12. Veloso N, Silva JD, Carvalho M, Rosa I, Medeiros I, Gon├¦alves L, et al. Endo-SPONGE┬« treatment for anastomotic leakage after colorectal surgery. GE J Port Gastrenterol 2013;20:132ŌĆō5.