- Search
| Ann Coloproctol > Volume 38(3); 2022 > Article |
|
Abstract
Hand-sewn anastomosis is an essential and fundamental skill for surgeons dealing with any gastrointestinal anastomosis. Despite the advances in minimally invasive surgery and stapling devices, there are still complex surgical circumstances when the surgeon’s surgical know-how are necessary. Therefore, a safe hand-sewn technique for bowel anastomosis is required to establish a tension-free, well-perfused, and sealed anastomosis that allows gastrointestinal continuity with no unexpected complications. We describe a step-by-step procedure for hand-sewn double-layered anastomosis that reflects these principles and is practical for small and large bowel anastomosis.
The constant evolution of minimally invasive surgery for colorectal cancer favors the development of advanced surgical devices and novel techniques aiming for better outcomes. Nevertheless, the surgeon’s knowledge, skills, and proficiencies still are an essential intraoperative resource, and there might be circumstances where a hand-sewn colon anastomosis is the best option [1]. Several unexpected events influence the choice of the anastomotic technique like diameter of bowel ends, contamination, accessibility, site of anastomosis, hemodynamic conditions, availability of time, and special equipment [2].
Lembert [3] proposed the construction of intestinal anastomoses in 1826, describing a double-layered mucosa inverting technique using suture bites with a 5-mm distance to the cut edge and a distance of 1 cm between sutures. In 1887, Halsted [4] stated the basis for a safe anastomosis: gentle handling of tissues, meticulous hemostasis, preservation of blood supply, strict aseptic technique, minimum tension on tissues, accurate tissue apposition, and obliteration of dead space. Since then, the principles for a successful bowel anastomosis have remained the same, leaving the surgeons to choose the most appropriate technique according to their individual surgical experience and personal preference.
Even though these principles have successfully translated to automatic stapling devices, surgeons must have a safe technique for hand-sewn anastomosis in their arsenal that fits the basic principles. The method for hand-sewn colorectal anastomoses is currently not standardized concerning inter-suture distance, suture distance to the anastomotic edge, interrupted or continue suture, and tension applied to it [5].
A meta-analysis including 2 randomized controlled trials and 4 nonrandomized studies compared the outcomes of stapled versus hand-sewn loop ileostomy closure, concluding there is no statistically significant difference in complications between stapled and sutured anastomoses, even though not being statistically significant, stapled anastomosis reported lower small bowel obstruction rates, anastomotic leaks and shorter operating times [6]. Dziki et al. [7] evaluated bowel anastomosis on day 28, demonstrating all hand-sewn anastomosis had larger diameters than the widest stapled anastomosis with greater mechanical strength, reduced tendency to stricture, and better histological healing. In a review conducted by Slieker et al. [5] in 2013, a single-layer continuous technique using inverting sutures with slowly absorbable monofilament material seems preferable, and distances of 5 and 10 mm from the cut edge will probably give adequate results.
Staple line reinforcement may positively prevent anastomotic leakage; however, it remains controversial and inconclusive as no robust data could demonstrate it [8]. Applying a coating layer of fibrin glue over the anastomotic line may protect the anastomosis from leakage, as reported in a retrospective case-control study conducted by Huh et al. [9] where fibrin glue was an independent factor of preventing anastomotic leakage in coloanal or low colorectal anastomosis in sphincter-preserving surgery for rectal cancer.
As another critical point, some authors had advocated that staplers were explicitly designed for bowels of normal thickness, and bowel edema might be an unsafe condition for stapled anastomosis due to slippage of the stapled mucosal and submucosal layer at a delayed time [10]. Bowel edema is usually a consequence of significant blood loss, prolonged surgeries, blood transfusions, hypotension, and hypothermia associated with the patient’s comorbidities [11]. However, in the context of emergency surgery, where unexpected findings and availability of special equipment might compromise the decision between hand-sewn anastomosis and stapled anastomosis, Demetriades et al. [6] did not find a significant difference in anastomotic leak rate or other abdominal complications.
We have described a technique that can be applied for side-to-side, end-to-end, and side-to-end anastomosis, with minimal changes in the sequence. The essential steps for hand-sewn and stapled bowel anastomosis are meticulous technique, good blood supply, and no tension [1]. The surgeon must evaluate the caliber difference between anastomotic lumens, bowel perfusion, and viability (by visual confirmation of pulsatile, bright red bleeding from the marginal artery, vascular flow confirmation by Doppler ultrasound, or use of indocyanine green induced fluorescence angiography) [12] and tension between segments, any alteration that suggests the risk of ischemia, rupture or asymmetry requires a change in the level of the planned anastomosis [13].
We introduce a double-layer hand-sewn bowel anastomosis technique, accompanied by a didactic dry lab simulation and live surgery video.
This note was approved by the Institutional Review Board of Yonsei University Health System (No. 2021-4098-001) and informed consent was obtained from the patients.
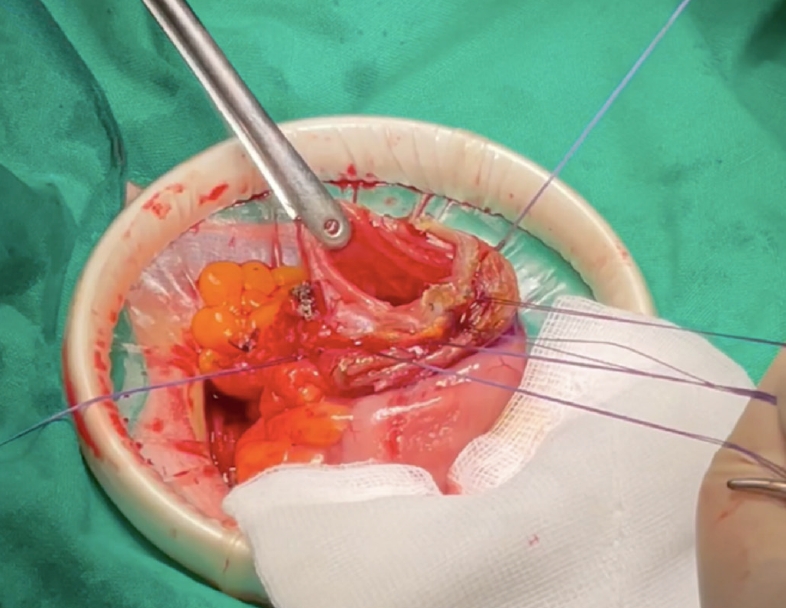
1. A posterior layer of interrupted seromuscular Lembert sutures is placed between the 2 anastomotic segments (Fig. 1).
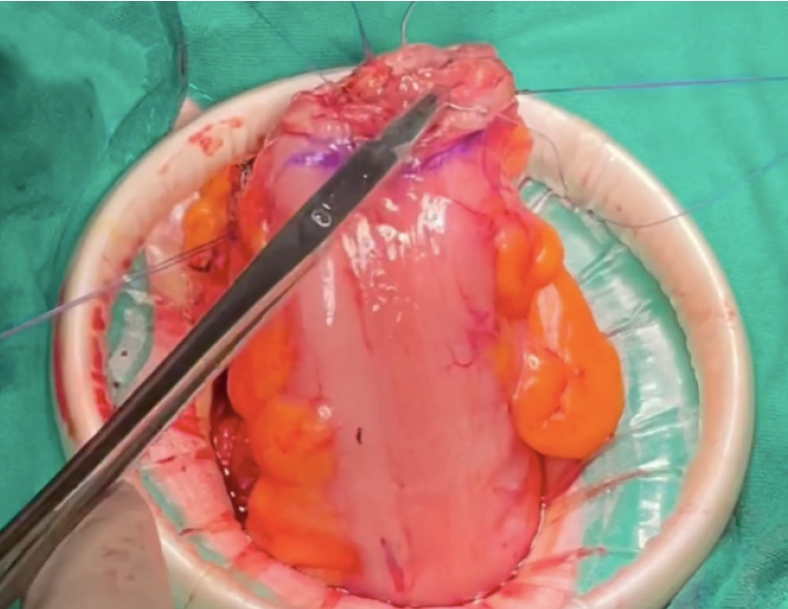
2. A longitudinal antimesenteric enterotomy is created in distal and proximal bowel ends (Fig. 2).
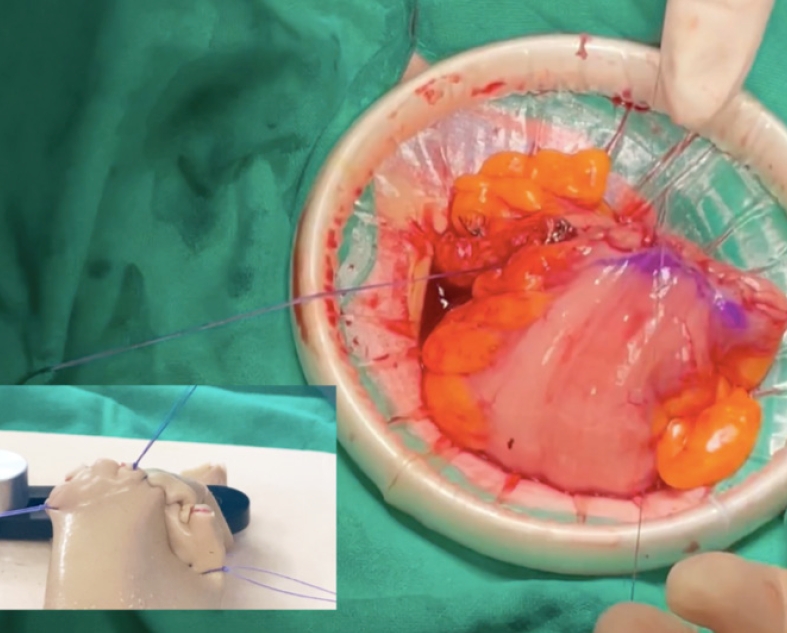
3. A full‐thickness interlocking continuous layer starts at the mid-point of the posterior wall and advances to the anastomotic angle (Fig. 3).
4. Angles are secured with full‐thickness interlocking continuous suture as the suture proceeds onto the anterior side of the anastomosis, inverting mucosa and continuing the anterior inner layer closure (Fig. 4).
5. Once the corners are passed and secured, the interlocking running suture continues to the middle of the anterior wall, where one or 2 final Connell stitches are taken to invert mucosa (Fig. 5).
6. With another 20-cm thread, a continuous full-thickness running suture is carried out starts from the opposite side of the bowel and progressing to the middle of the anterior wall following the same steps (Fig. 6).
7. Sutures’ ends are tied after meeting in the middle of the anterior wall (Fig. 7).
8. The anterior and posterior suture lines are oversewn with interrupted seromuscular inverting Lembert sutures (Fig. 8).
• Absorbable suture (braided or monofilament 3-0 taper point) is advised for all steps.
• This sequence of steps is advised for side-to-side, end-to-end, and side-to-end anastomosis (See Supplementary Video 1 for technical differences).
• In the case of an open intestinal lumen after sharp resection, enterotomy will not be necessary after suturing the posterior wall. Surgeons must prevent the leakage of intestinal contents.
• Blood perfusion of anastomotic segments can be assessed by the evidence of rutilant mucosa bleeding after enterotomy.
• Full-thickness interlocking running suture—including submucosa—guarantees a hemostatic and airtight anastomosis.
• Although the posterior side of the anastomosis is initially sutured, it is advised to double-check as a final step and use interrupted Lembert sutures if needed to reinforce specific points.
• The assistant must ensure tension to the thread to enable a tight suture line. This can be enhanced by using a small wet gauze to press along the puncher site.
• The diameter of the bowel lumen after anastomosis should always be checked by digital palpation.
In conclusion, double-layered hand-sewn anastomosis is a feasible bowel anastomosis method in elective and emergency surgery. The anastomotic technique selected depends on the site of anastomosis, bowel caliber, quality, and underlying disease process. The mechanical strength of the anastomosis is essential to make a watertight and airtight anastomosis free from leakage, no matter by hand-sewn or by staplers.
SUPPLEMENTARY MATERIAL
Supplementary materials for this study are presented online (available at https://doi.org/10.3393/ac.2021.00990.0141).
Fig. 1.
A posterior layer of interrupted seromuscular Lembert sutures is placed between the 2 anastomotic segments.

Fig. 3.
A full‐thickness interlocking continuous layer starts at the mid-point of the posterior wall and advances to the anastomotic angle.

Fig. 4.
Angles are secured with full‐thickness interlocking continuous suture as the suture proceeds onto the anterior side of the anastomosis, inverting mucosa and continuing the anterior inner layer closure.
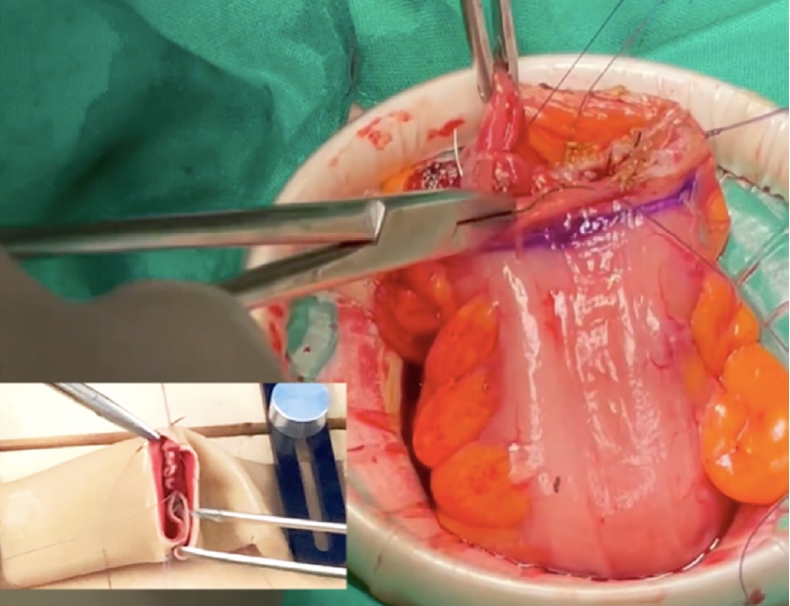
Fig. 5.
Once the corners are passed and secured, the interlocking running suture continues to the middle of the anterior wall, where one or 2 final Connell stitches are taken to invert mucosa.

REFERENCES
1. Goulder F. Bowel anastomoses: the theory, the practice and the evidence base. World J Gastrointest Surg 2012;4:208–13.



2. Choy PY, Bissett IP, Docherty JG, Parry BR, Merrie AE. Stapled versus handsewn methods for ileocolic anastomoses. Cochrane Database Syst Rev 2007;(3):CD004320.

3. Lembert A. Memoire sur l’enteroraphie avec la description d’un procede nouveau pour pratiquer cette operation chirurgicale. Rep Gen Anat Physiol Path 1826;2:100–7.
4. Halsted WS. Circular suture of the intestine: an experimental study. Am J Med Sci 1887;94:436–61.

5. Slieker JC, Daams F, Mulder IM, Jeekel J, Lange JF. Systematic review of the technique of colorectal anastomosis. JAMA Surg 2013;148:190–201.


6. Demetriades D, Murray JA, Chan LS, Ordoñez C, Bowley D, Nagy KK, et al. Handsewn versus stapled anastomosis in penetrating colon injuries requiring resection: a multicenter study. J Trauma 2002;52:117–21.


7. Dziki AJ, Duncan MD, Harmon JW, Saini N, Malthaner RA, Trad KS, et al. Advantages of handsewn over stapled bowel anastomosis. Dis Colon Rectum 1991;34:442–8.


8. Leung TT, MacLean AR, Buie WD, Dixon E. Comparison of stapled versus handsewn loop ileostomy closure: a meta-analysis. J Gastrointest Surg 2008;12:939–44.


9. Huh JW, Kim HR, Kim YJ. Anastomotic leakage after laparoscopic resection of rectal cancer: the impact of fibrin glue. Am J Surg 2010;199:435–41.


10. Brundage SI, Jurkovich GJ, Grossman DC, Tong WC, Mack CD, Maier RV. Stapled versus sutured gastrointestinal anastomoses in the trauma patient. J Trauma 1999;47:500–8.


11. Alves A, Panis Y, Trancart D, Regimbeau JM, Pocard M, Valleur P. Factors associated with clinically significant anastomotic leakage after large bowel resection: multivariate analysis of 707 patients. World J Surg 2002;26:499–502.