Anal Gland/Duct Cyst: A Case Report
Article information
Abstract
Anal gland/duct cyst (AGC) is rare and observed in only 0.05% of patients undergoing anal surgery. AGC is thought to be a retention cyst in the anal gland and arises when an obstruction of the anal duct causes fluid collection in the anal gland. We report a case of AGC in a 66-year-old woman without anal symptoms. Found by colonoscopy, the AGC was excised transanally. The histopathology of the specimen confirmed AGC. Colonoscopists should include AGC in the differential diagnosis of anal canal mass and rule out of malignancy. Excision is recommended for definitive diagnosis and treatment.
INTRODUCTION
Anal gland/duct cyst (AGC) is one of the cysts that are found in the perianal region and anal canal. Perianal cysts are uncommon and seen in only 0.05% to 0.06% of patients who undergo anal surgery [1, 2]. AGC is thought to be a retention cyst in the anal gland and arises when an obstruction of the anal duct causes fluid collection in the anal gland [3]. There are some reports of AGC in the foreign literature, but few are published in Korea, especially in English. Here, we report a case of AGC that was detected by colonoscopy in a patient without anal symptoms.
CASE REPORT
A 66-year-old woman visited our clinic with a history of loose stools without anal symptoms. Her past medical history and family history were unremarkable. The laboratory blood tests, including white blood cell count, hemoglobin, platelets, alanine aminotransferase, and aspartate transaminase, were within the normal limits. A viral marker for hepatitis B and a serologic investigation for the immunocompromised state (HIV antibody) were negative. The patient underwent a colonoscopy which revealed an approximately 5-mm-sized, yellowish, submucosal tumor in the anal canal (Fig. 1). On digital rectal examination, a 5-mm-sized, hard, movable tumor was palpated in the anterior wall of the anal canal. The patient was anesthetized with a caudal block, and the tumor was excised using a transanal approach. The histopathology of the specimen revealed AGC, and microscopic examination showed a cystic lesion lined by squamous epithelium and glandular tissue composed of columnar epithelium in the lumen (Fig. 2). The patient’s postoperative course was uneventful, and she was discharged on postoperative day 3. No recurrence was observed after 6 months of follow-up.
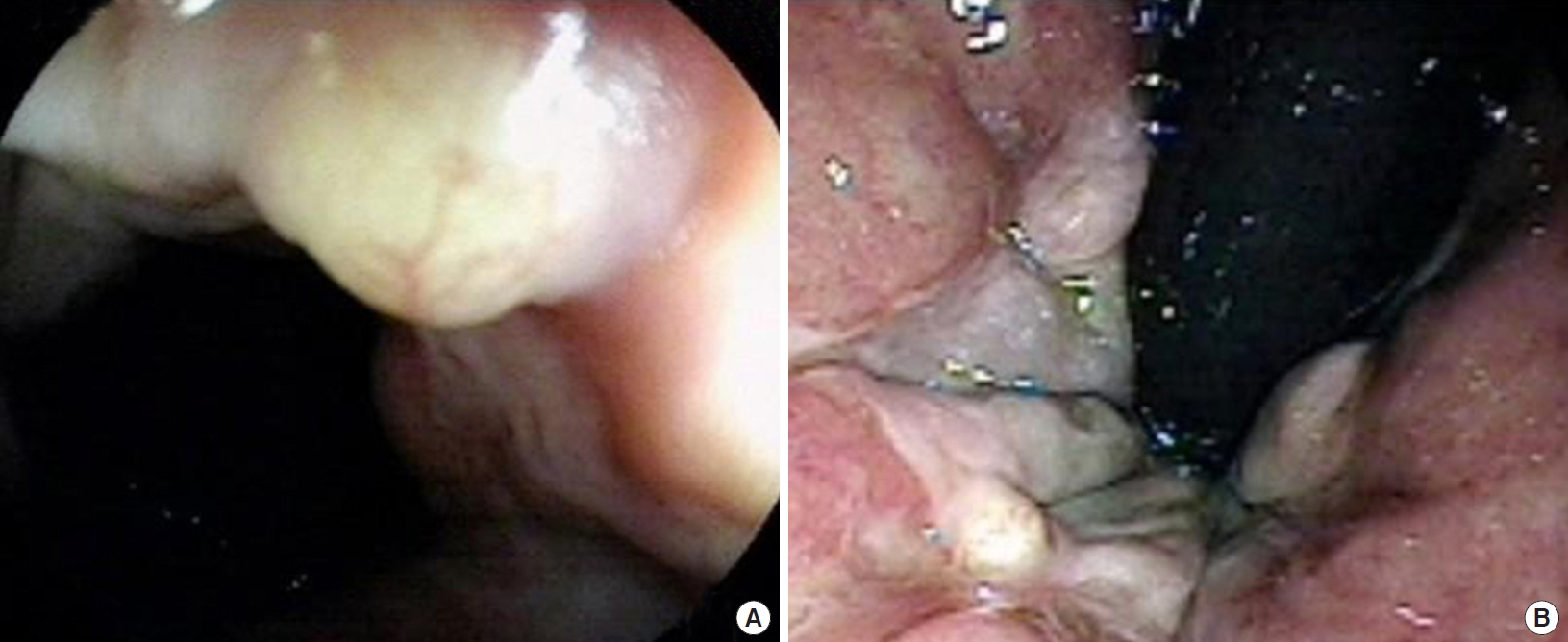
Anal gland/duct cyst in a 66-year-old female. Yellowish polypoid lesion was demonstrated under colonoscopic examination (A) and reversed view (B).
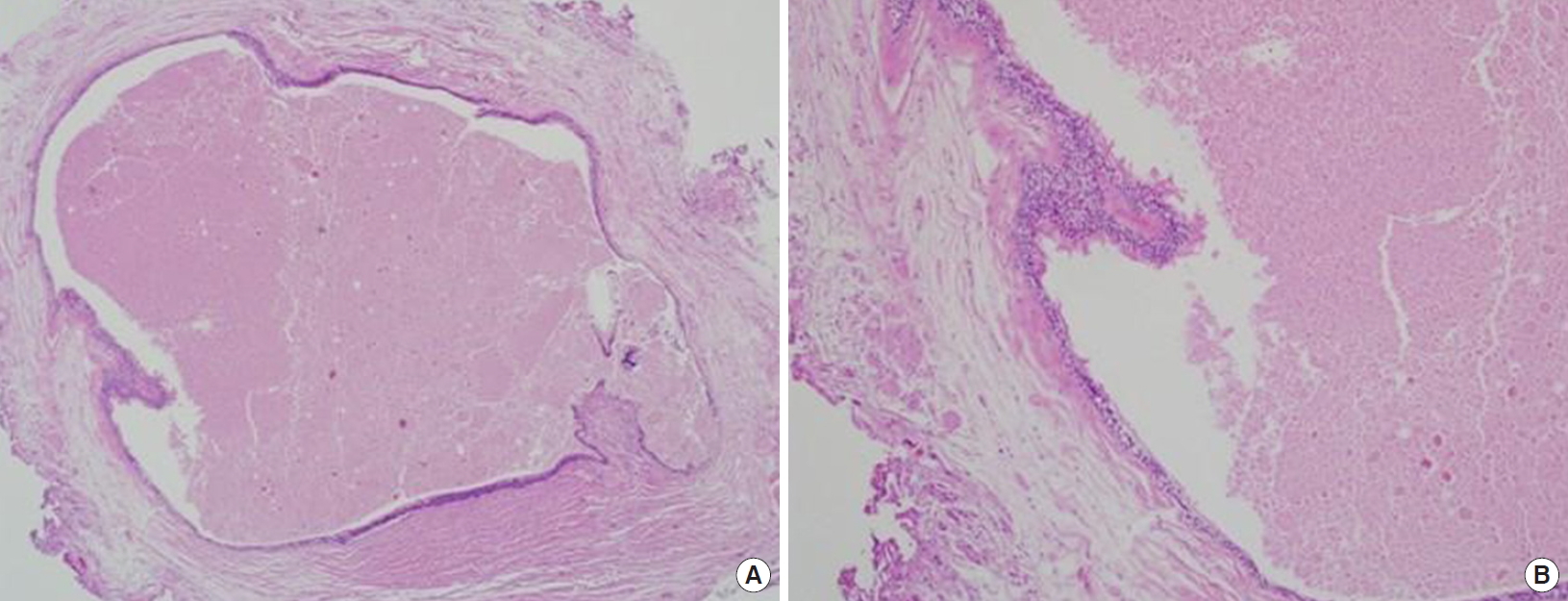
(A) Microscopic examination revealed a cystic lesion lined by squamous epithelium and fluid collection in the center of the lumen (H&E, ×40). (B) Glandular tissue composed of columnar epithelium in the lumen (H&E, ×100).
Written informed consent was obtained from the patient for publication of this case report and accompanying images. This study was approved by the electronic Institutional Review Board of the Korea National Institute for Bioethics Policy (KoNIBP) (IRB No. P01-201807-21-012).
DISCUSSION
AGC is one of the rare perianal cysts and occurs in about 0.05% of patients undergoing anal surgery [1, 2]. Arising when an obstruction of the anal duct causes fluid collection in the anal gland, AGC is considered to be a retention cyst in the anal gland [1, 3]. In one report, AGC presented as a lump at the anus or was discovered on a rectal examination or at the time of surgery for some other condition [4]. In our case, the cyst was found during colonoscopy as a submucosal tumor in the anal canal, and it was located in the anterior midline of the anal margin.
Arakawa and Arakawa [1] summarized 10 cases of perianal cysts related to anal ducts, and 8 cases (80%) had an anterior location. Similarly, Ozawa et al. [2] reported 6 patients with perianal cysts; 5 cases (83.3%) were AGC and 4 cases (66.7%) were located in the anterior midline of anus. Therefore, AGCs seem to occur on the anterior wall of the anus. The patient’s AGC in our case was located on the anterior wall of the anus in the anal canal, although AGCs can occur at the presacral, precoccygeal, and retrorectal spaces.
Diagnosis of anal gland cyst is based on the histological characteristics of mucus and/or the presence of a communication with the anal duct or crypt [5]. Based on these criteria, Kulaylat et al. [5] suggested that some of the reported cases of mucus-secreting cysts occurring around the anorectum may prove to be anal gland/ducts in origin. The authors also think that cysts classified as mucus secretion cysts in past reports may be anal gland cysts.
In general, infections around the anus are common, but tumors and cysts around the anus are uncommon. However, tumors and cysts of the perianal region commonly occur in the presacrococcygeal space [6], and Kulaylat et al. [5] reported a case of AGC in the retrorectal space. The perianal region, a wide and ambiguous range, includes the internal and external region of the anus, and perianal cysts include other cysts, such as tailgut, dermoid, epidermoid, and teratomas, which occur in the presacral or retrorectal space [2, 5-8]. The presacral space, often referred to as the retrorectal space, is a potential space that lies anterior to the sacrum and coccyx, and its inferior boundary is the levator ani and coccygeal muscle [8]. Therefore, the retrorectal tumors of perianal cysts are frequently unrecognized, misdiagnosed, and treated by variable approaches, but they need to be an important of the differential diagnosis [7]. However, McColl [4] reported 31 cystic lesions arising from the anal glands that were limited to the anal canal and rectum, and these occurred at 2 sites: the perianal region and the presacral region. We think physicians should separately consider the cysts which occur in these 2 distinct locations, because the treatment approach and prognosis differ depending on the location. That is, cysts that occur in the lower part of the anus and anal canal are easier to treat and access surgically.
In previous reports [3, 9], the AGC was endoscopically resected, but we surgically resected the AGC in the present case. Although it seemed to be a cystic tumor during colonoscopy, we could not rule out the possibility of malignancy, so we chose a transanal resection to allow a more accurate resection margin than endoscopic resection. As a result of electrocautery, it is sometimes difficult to accurately evaluate tumor resection margins during endoscopic resection. Furthermore, it is difficult to visualize the interior of the anal canal during endoscopic resection, and resection below the dentate line can be painful [3]. In our experience, endoscopic resection is limited by technique and equipment.
Our case was incidentally found in a patient without anal symptoms, but Uchimot et al. [3] and Park et al. [9] reported patients with anal bleeding and fecal incontinence, respectively. There is no mention of recurrence or follow-up visits in the previous literature. But, in our case, there was no recurrence at 6 months follow-up. To our knowledge, there is one case report of an endoscopically-resected AGC in Korea [9], but only the abstract is in English, and the text is written in Korean. We think our case report is the first English manuscript describing an AGC in Korea.
Like this case, Park et al. [9] reported a submucosal tumor in the anal canal, and it was necessary to distinguish it from carcinoid tumor. Although AGC is a rare benign cyst, it requires differentiation from other cysts, such as epidermoid, dermoid, tailgut, teratoma, and anal abscess [7, 9]. There are some documents that report a malignant case arising from an anal gland or anal duct [10, 11]. So, excision is necessary for diagnosis and treatment.
In conclusion, we report a case of AGC that was detected by colonoscopy in the anal canal of a patient without anal symptoms. Colonoscopists should include AGC in the differential diagnosis of an anal canal mass and rule out of malignancy. Excision is recommended for definitive diagnosis and treatment.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
