Treatment of side limb full-thickness prolapse of the side-to-end coloanal anastomosis following intersphincteric resection: a case report and review of literature
Article information
Abstract
Intersphincteric resection (ISR) with coloanal anastomosis is an oncologically safe anus-preserving technique for very low-lying rectal cancers. Most studies focused on oncological and functional outcomes of ISR with very few evaluating long-term postoperative anorectal complications. Full-thickness prolapse of the neorectum is a relatively rare complication. This report presents the case of a 70-year-old woman presenting with full-thickness prolapse of the side limb of the side-to-end coloanal anastomosis occurring 2 weeks after the stoma closure and 2 months after a robotic partial ISR performed with the Da Vinci single-port platform. The anastomosis was revised through resection of the side limb and conversion of the side-to-end anastomosis into an end-to-end handsewn anastomosis with interrupted stitches. This study describes the first case of full-thickness prolapse of the side limb of the side-to-end handsewn coloanal anastomosis following ISR. Moreover, a revision of all reported cases of post-ISR full-thickness and mucosal prolapse was performed.
INTRODUCTION
Intersphincteric resection (ISR) with coloanal anastomosis is an oncologically safe anus-preserving technique for very low-lying rectal cancers (within 5 cm from the anal verge [AV]) [1–3]. ISR is a safe oncological alternative to abdominoperineal resection (APR) with permanent colostomy [1]. Most studies on ISR focused on oncological and functional outcomes with very few evaluating long-term postoperative anorectal complications [4, 5].
Most common anorectal complications of ISR are external hemorrhoids, anal stenosis, and full-thickness/mucosal prolapse (FMP) of the neorectum [4, 6]. FMP is a relatively rare complication (incidence, 4.1%–14.8%) [2, 4, 6]. Pathophysiology of FMP is unknown; however, Kuo et al. [4] postulated that pressure differences between the anal canal and the abdominal cavity could result in an intussusception of the colon which could be aggravated by the impaired function of the remnant anal sphincter complex. Also, patient’s pelvic anatomy (shallow pelvis, short anal canal) could predispose to FMP [4]. Increasing age (leading to pelvic floor muscle weakness) and lifestyle changes can also be considered as risk factors. Although ISR itself cannot be considered as a risk factor for FMP, some authors reported that total ISR and shortening distance of coloanal anastomosis can be, while others disagree on the role of ISR extension (total vs. partial) [5].
Signs and symptoms of FMP are pain, bulge sensation in the anus, worsened anal function, constipation, diarrhea, soling, fragmentation, mucus discharge, urgency, and bleeding during defecation [5, 7]. Local relapse should be excluded and sphincter tone should be assessed when diagnosing an FMP, after an oncological resection, and before considering a surgical treatment.
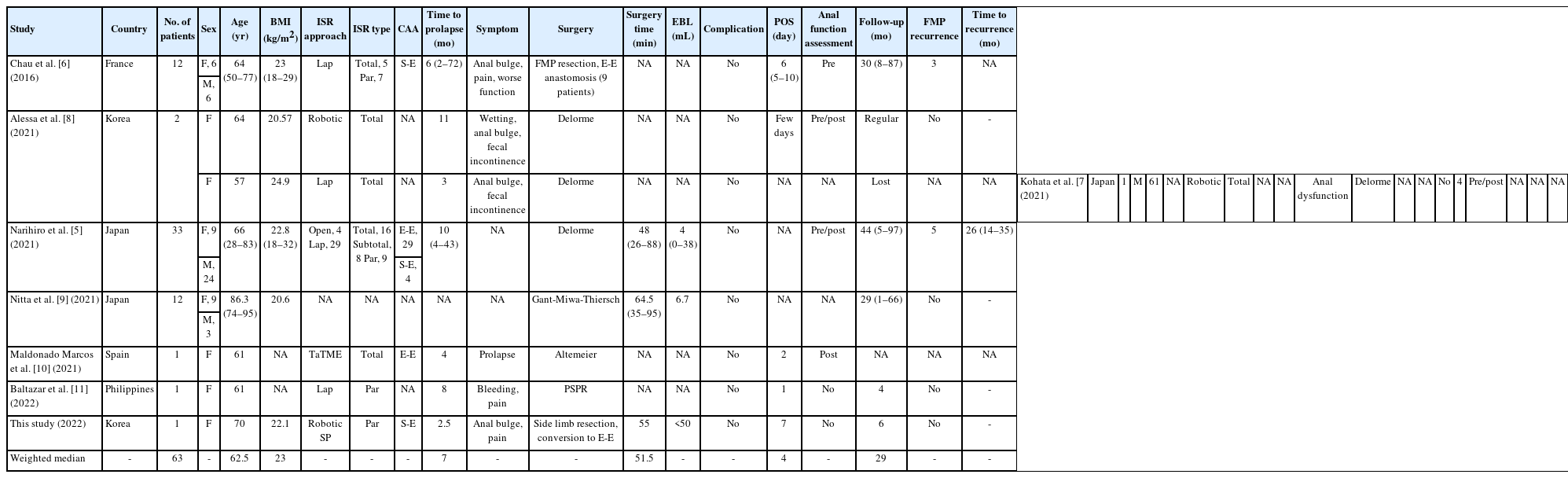
FMP has no standard treatment with several techniques, preserving the sphincter function and avoiding a definitive colostomy, as reported in the literature (Table 1) [5–11].
Here, we report the first case of FMP of the side limb of the side-to-end handsewn coloanal anastomosis following ISR with ileostomy closure. We also revised the literature on FMP in order to outline the main characteristics and surgical treatment of an underreported complication.
CASE REPORT
A 70-year-old woman with a body mass index (BMI) of 22.1 kg/m2 was diagnosed with a low rectal cancer located 2.5 cm from the AV causing anal pain. Endoscopic biopsy showed a moderately differentiated adenocarcinoma. Clinical staging with pelvic magnetic resonance imaging showed a 3.7 cm right-sided ulcerofungating lesion with a suspicious invasion of the levator ani muscle (mrT4N0M0).
The patient underwent neoadjuvant chemoradiotherapy (nCRT; 50 Gy in 28 fractions with concurrent oral capecitabine). Clinical restaging on magnetic resonance imaging showed no radiologic evidence of residual viable tumor and no enlarged lymph nodes (ymrT0N0M0, mrTRG1). Colonoscopy showed a complete response.
The patient was submitted to robotic partial ISR with side-to-end handsewn coloanal anastomosis and loop ileostomy with the Da Vinci single-port (SP) platform (Intuitive Surgical System Inc) [12]. The surgery was uneventful and lasted 210 minutes. Estimated blood loss was <50 mL. The postoperative course was uneventful and the patient was discharged on postoperative day 8 in good general conditions. The final pathological exam showed ypT0N0 (0/22) with no evidence of disease at the levator ani muscle (intraoperative biopsy). The scar lesion was 3.2×2.0 cm with a distal resection margin of 0.1 cm. The lesion showed a grade 1 regression after nCRT according to Thies and Langer [13]. Loop ileostomy was closed 2 months later.
Two weeks later the patient reported a sense of intermittent anal bulge associated with pain. Fecal continence was tolerable with frequent small discharges. Physical examination showed a full-thickness prolapse (Fig. 1). Digital rectal examination reported a weak anal sphincter tone with full-thickness prolapse. The prolapse was referred to be worsened by standing and walking and to resolve when lying down. Medication with antidiarrheal and analgesic improved the bowel movements however was not fully effective. A Delorme procedure was planned.
The patient underwent intraoperative inspection under general anesthesia in the lithotomy position (Fig. 2A). This showed total prolapse of the side limb of the side-to-end handsewn coloanal anastomosis (Fig. 3A, B). The original indication was changed following the recognition of prolapse of only the side limb and not the true luminal mucosa. The anastomosis was revised through resection of the side limb (Figs. 2B, 3C) and conversion of the side-to-end anastomosis into an end-to-end handsewn anastomosis with interrupted stitches (Figs. 2C, 3D). The mesentery was carefully resected to avoid ischemic injury of the anastomosis. Colonic mucosal color was healthy at the end of the resection and interrupted suture (Fig. 2D). Estimated blood loss was <50 mL. The surgery lasted 55 minutes. Postoperatively the mucosal color was adequate. The patient referred anal pain which was controlled with medication. Oral diet was permitted on day 4. The patient was discharged on the 7th postoperative day in good general condition and is currently in follow-up.
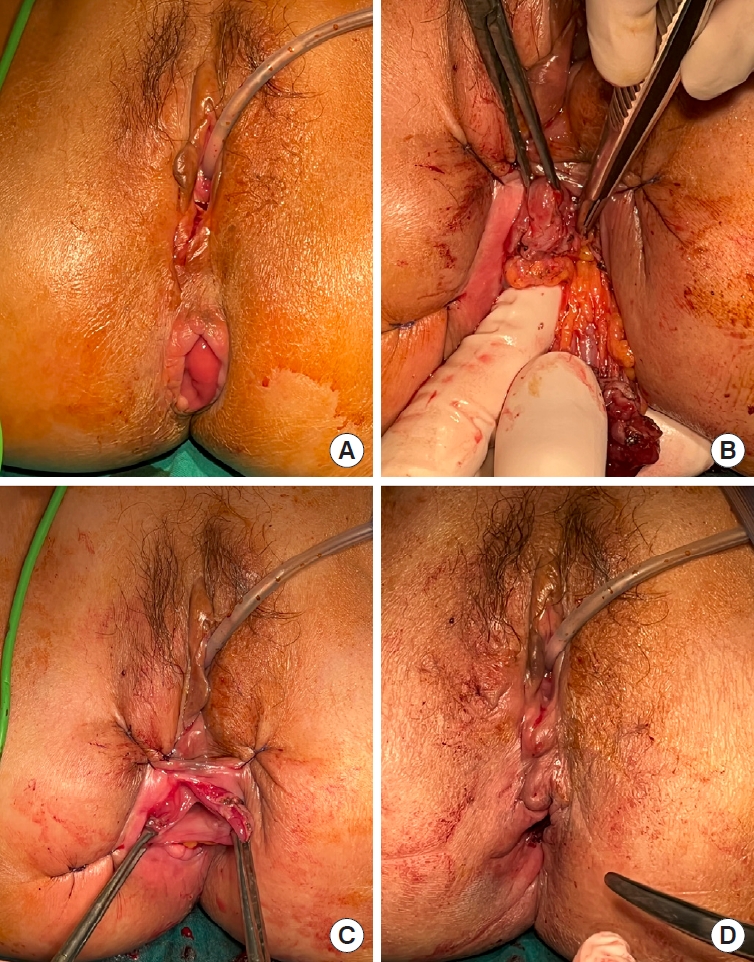
Intraoperative images. (A) Preoperative view of the full-thickness prolapse after induction of general anesthesia (see Fig. 3B). (B) Resection of the side limb of the side-to-end coloanal anastomosis (see Fig. 3C). (C) Conversion of the side-to-end anastomosis into an end-to-end handsewn anastomosis with interrupted stitches (see Fig. 3D). (D) Final view.
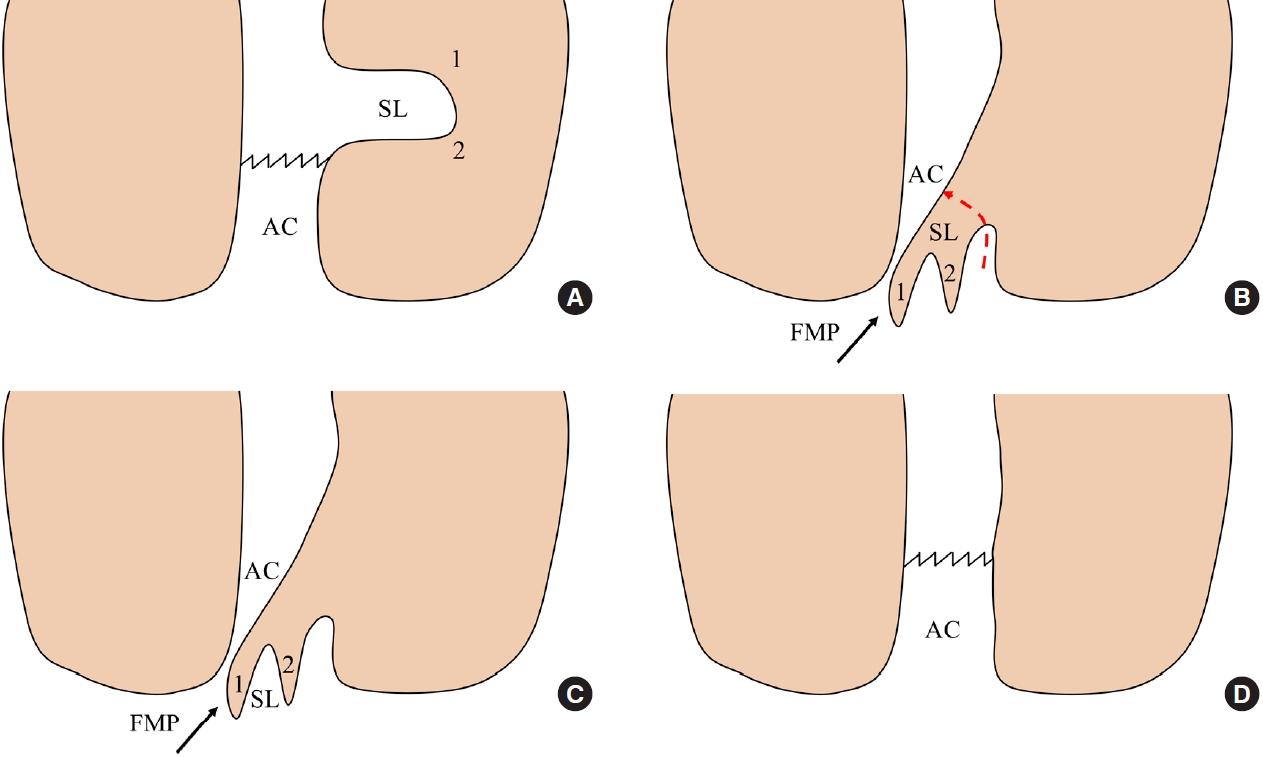
Simplified technical schemes from an anteroposterior view. (A) Scheme of a side-to-end coloanal anastomosis (anal canal [AC] and side limb [SL]). (B) Full-thickness prolapse (FMP) of the SL of the side-to-end coloanal anastomosis (numbers 1 and 2 help in showing the prolapsed sections, see Fig. 2A). (C) Transanal resection (red dotted line) of the SL of the side-to-end coloanal anastomosis (see Fig. 2B). (D) Conversion of the side-to-end anastomosis into an end-to-end handsewn anastomosis (see Fig. 2C, D).
Ethics statement
This study was conducted in compliance with the principles of the Declaration of Helsinki. Written informed consent for publication of the research details and clinical images was obtained from the patient.
DISCUSSION
Since its first description in 1994 by Schiessel et al. [14], several reports have evaluated the oncological and functional outcomes of ISR with little interest in the long-term complications. However, being ISR a complex technique with extensive pelvic dissection, long-term complications should be carefully evaluated and reported regularly.
Up to date, only 7 reports have described the outcomes and treatments of FMP after ISR (Table 1) [5–11], while Kuo et al. [4] have reported the long-term complications altogether from a series of 108 robotic ISR cases (16 FMP cases, 14.8%). However, they did not describe the FMP cases thoroughly so were not considered in the current review. Six studies were published in the last 2 years showing a growing interest in FMP, especially in East Asia (Japan and Korea). The widest studies were from Narihiro et al. [5] (33 cases from a total of 720 ISRs; incidence, 4.5%), Nitta et al. [9] (12 cases), and Chau et al. [6] (12 cases, of which 9 treated surgically). Together with the current study, a total of 63 cases of FMP were reported in detail. Male sex was predominant (34 cases, 54.0%). The median age was 62.5 years (range, 28–95 years) while the median BMI was 23 kg/m2 (range, 18–32 kg/m2).
ISR was performed with open (4 cases), laparoscopic (33 cases), transanal (1 transanal total mesorectal excision), multiport robotic (2 cases), and SP robotic approach with the Da Vinci SP platform (1 case) [12]. Primary ISR was partial (18 cases), subtotal (8 cases), and total (25 cases). This shows that FMP can occur with any level of internal anal sphincter excision. The primary coloanal anastomosis was end-to-end in 30 cases and side-to-end in 6 cases. Interestingly, the median time to FMP was only 7 months (range, 2.5–72 months); therefore, this complication should be easy to report in routine surgical follow-up.
Local symptoms of FMP included pain, bleeding during defecation, soiling or discomfort in the anus, mucosal bulge, and fecal incontinence which affected the quality of life.
Surgery is the only definitive and curative treatment option for rectal prolapse and can be performed both transabdominally or perineally. However, the transabdominal approach would be extremely challenging in the case of FMP following ISR because of the dense adhesions in the pelvis. Therefore, a perineal approach (Delorme, Altemeier, and Gant-Miwa-Thiersch procedure) should be considered the best first choice.
Delorme procedure was the most offered to treat FMP (3 studies) [5, 7, 8], followed by Altemeier (1 study) [10], Gant-Miwa-Thiersch (1 study) [9], perineal stapled prolapse resection (PSPR; 1 study) [11], FMP resection and end-to-end anastomosis (1 study) [6], and side limb resection and conversion to end-to-end anastomosis (1 study).
Surgical time and estimated blood loss were reported only by 3 reports [5, 9]. No complications were reported in any series. Median postoperative hospital stay was 4 days (range, 1–10 days).
Narihiro et al. [5] reported that the Delorme procedure, through the reconstructive stitches at the muscular layer after mucosal excision, can provide a sphincter-like function mimicking the internal anal sphincter. This increases the maximal resting pressure and maximal voluntary contraction pressure and decreases the minimum expression of feces and the maximum tolerated dose. These functional improvements could derive also from the recovery of the anal sphincter tone following the removal of the prolapsed rectum which could be stretching and attenuating its fibers. The authors compared the preoperative and postoperative Wexner scores of patients whose diverting stoma were closed before Delorme procedure, reporting a change from 15.1 (range, 6–20) to 12.9 (range, 2–20) which was close to the Wexner score of patients submitted to ISR with no FMP (9 at 2 years and 8.5 at 5 years) after stoma closure [15]. Moreover, perineal symptoms improved in all 33 patients [5].
Alessa et al. [8] reported the functional benefit in one patient undergoing Delorme procedure (Wexner score, from 20 to 18; Memorial Sloan Kettering Cancer Center bowel function instrument, from 57 to 52).
Only Kohata et al. [7] performed an anal function assessment preoperatively and postoperatively after Delorme procedure with anorectal manometry showing that maximum resting pressure remained low (13.2–18.0 mmHg), while the maximum squeeze pressure score changed from 214 to 350 mmHg.
Nitta et al. [9] described the Gant-Miwa procedure, which is a plication technique for herniated rectal mucosa characterized by the formation of multiple nodules in the sutured mucosa through a transfixing suture, followed by the Thiersch procedure, which is characterized by the narrowing of the anal canal using a 1 nylon suture placed around the anal orifice in the subcutaneous plane.
Maldonado Marcos et al. [10] reported an Altemeier procedure with an acceptable postoperative low anterior resection score of 23.
The PSPR was reported to have comparable outcomes to Delorme and Altemeier procedures, with a recurrence rate of 0%–44% in patients with a follow-up of more than 12 months compared to 0%–31.3% of Altemeier and Delorme altogether [16], and 23.8%–51% of Gant-Miwa procedure [5]. PSPR technique was reported to improve functional outcomes (Wexner continence score and the obstructed defecation syndrome score) [17]. The advantage of PSPR is its technical simplicity and reproducibility [11]. In fact, PSPR does not require extensive and fine perineal dissection which is dependent on the surgeon’s experience and expertise in perineal surgery. PSPR is a faster and less challenging technique; however, a major disadvantage is the added cost of the staplers [16].
Median follow-up was 29 months (range, 4–97 months). During follow-up, only 2 studies [5, 6] reported symptom recurrence with only 1 study [5] reporting time to recurrence.
Chau et al. [6] reported an FMP recurrence of 33% (3 cases) after a median follow-up of 30 months (range, 8–87 months). Recurrences were diagnosed on clinical examination and/or symptoms occurrence as anal pain while sitting and worsening fecal incontinence. One patient with bad function was submitted to APR and definitive stoma, while the other 2 underwent successful reoperation with the same procedure. Therefore, 8 of 9 patients (89%) were successfully treated for FMP with functional improvement.
The absence of a shared standard technique for FMP derives both from low reporting of this complication and from absence of multicenter studies with wide series on ISR. Delorme procedure, being a well-known transanal technique for colorectal surgeons, could be the best-shared option in an expert center, while the PSPR could be a good option for less-specialized surgeons. However, FMP after ISR can be very variable with the need for patient-tailored surgery as for our case of side limb prolapse of a side-to-end coloanal anastomosis. New multicenter studies on ISR are needed aiming to collect long-term follow-up data on complications and surgical treatment.
This study describes the first case of full-thickness prolapse of the side limb of the side-to-end handsewn coloanal anastomosis following ISR. Moreover, a revision of all reported cases of post-ISR FMP was performed. All perineal techniques share similar benefits on postoperative outcomes, symptom relief, and reduced risk of FMP recurrence. There is no shared standard technique for FMP. Further prospective multicenter studies on ISR are needed with special reporting on long-term perineal complications.
Notes
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Funding
None.
Author contributions
Conceptualization: GNP, KK. Data curation: GNP, KK, SHS, JMC. Methodology: GNP, KK. Formal analysis: GNP, KK; Investigation: GNP, KK; Supervision: SHK; Writing–original draft preparation: GNP, KK; Writing–review & editing: SHK. All authors read and approved the final manuscript.