- Search
| Ann Coloproctol > Epub ahead of print |
|
Abstract
Juvenile polyps (JPs) are the most common polyps in pediatric patients. We present the case of an 18-year-old male patient with a giant solitary JP resembling solitary rectal ulcer syndrome (SRUS). The presenting history was rectal bleeding and symptoms of obstructed defecation syndrome. Colonoscopy revealed a polypoidal mass at the anorectal junction, with biopsy-confirmed SRUS. The symptoms worsened, and a protruding mass from the anus caused fecal incontinence. Pelvic magnetic resonance imaging showed a huge pedunculated mass occupying the low rectum with local compression of the urinary bladder. Transanal excision of the anal tumor was performed due to bleeding. A histopathological examination showed a JP with high-grade dysplasia. A histological examination to differentiate JPs and SRUS could be challenging based on a superficial forceps biopsy. Therefore, an excision biopsy is usually warranted with the understanding that adenomatous or malignant transformation is found in 5.6% to 12% of all JPs.
Juvenile polyps (JPs), which are the most common type of polyps found among pediatric patients, consist of juvenile polyposis syndrome or simple JPs [1, 2]. Typical presentations include painless rectal bleeding, mucoid stool, and a mass protruding through the anus [3]. The most frequent location for JPs is the rectosigmoid colon, although they can also be distributed in the left, transverse, and right colon [2]. Herein, we report a case of a giant solitary anal JP with an initial presentation of obstructed defecation syndrome (ODS) with solitary rectal ulcer syndrome (SRUS) that eventually progressed to a worrisome bleeding polyp with incontinence.
An 18-year-old man presented with intermittent rectal bleeding and mucoid stool for the past year. His symptoms were consistent with ODS, which involves excessive straining, incomplete evacuation, and digital manual evacuation of feces. He was investigated thoroughly with gastroscopy and colonoscopy before being referred to our center. Gastroscopy was unremarkable, while colonoscopy showed a polypoidal lesion at the low rectum with biopsy-confirmed SRUS. He was prescribed laxatives and enemas; however, the ODS symptoms persisted without improvement (Renzi obstructed defecation score, 16/20). The rectal bleeding became more worrisome; hence, he underwent another colonoscopy with similar findings and a repeated biopsy-confirmed SRUS. He was managed conservatively with laxatives and diet modification while waiting for anal manometry.
During subsequent follow-up, after 6 months, he complained of a mass protruding from the anal canal during each defecation but stated that the mass was easily digitally reducible. Despite the reduction, he experienced frequent soiling and incontinence. His Jorge-Wexner incontinence score was 15 (out of 20). Diapers had become part of his daily life apparel, which was stigmatizing. A digital rectal examination showed a polypoidal mass 3 cm proximal to the anal verge. Sigmoidoscopy revealed a huge pedunculated polypoidal mass with contact bleeding (Fig. 1). Pelvic magnetic resonance imaging was performed and revealed a benign well-defined lobulated mass with its long stalk arising from the anal canal, occupying the rectum and compressing the urinary bladder (Fig. 2).
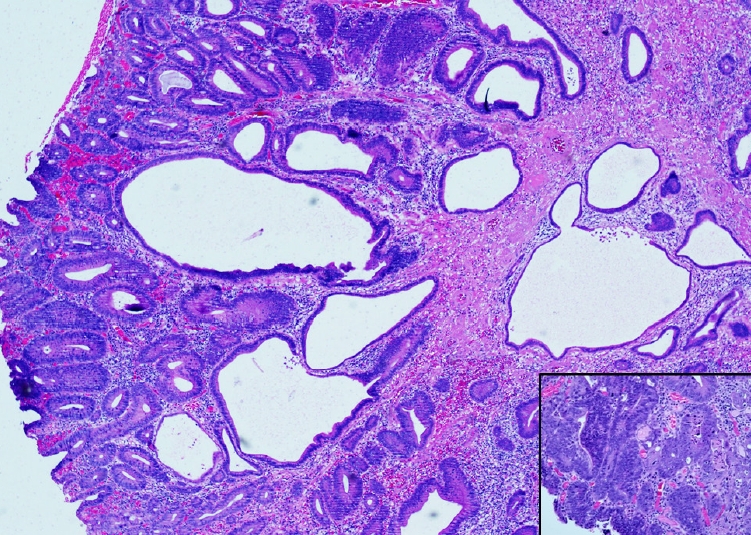
Transanal resection of the rectal tumor was performed. During an examination under anesthesia, the mass extruded out from the anal canal prior to resection (Fig. 3A). The anorectal junction with the low rectal mucosa could be seen prolapsing out, suggesting that the base of the polyp was located at the anorectal junction. A stay-suture was applied to the anorectal mucosa surrounding the mass, and excision was carried out with caution, preserving the internal anal sphincter. The tumor, which constituted a broad-based polypoidal mass arising at the anorectal junction, was excised entirely (Fig. 3B). The final resected specimen demonstrated intact muscularis mucosa without a perpendicular extension into the crypts, which was suggestive of JP instead of SRUS. Moreover, we noted high-grade dysplasia, which was absent in SRUS in the previous biopsy (Figs. 4, 5). Postoperatively, his symptoms resolved entirely, and his quality of life improved. At a 3-month follow-up, the patient indicated that he no longer experienced soiling and his continence was completely restored.
JPs are the most common polyps detected in children. Almost all of the polyps (80%ŌĆō100%) removed from children on colonoscopy are JPs, while the others are found in cases of either familial adenomatous polyposis or Peutz-Jegher syndrome [3]. In a survey of endoscopic findings among children, JPs were divided into solitary JPs, multiple JPs, or juvenile polyposis syndrome, with solitary JPs being most commonly seen in younger children [3, 4]. JPs are most commonly found in the rectosigmoid colon, while they can also be found in the left, transverse, and right colon in descending order [5]. Multiple publications have described different colonic sites for JPs; however, none reported cases in the anal canal, and solitary JPs in the anal canal are even rarer.
The most common clinical presentations are painless rectal bleeding, a prolapsed mass from the rectum, mucoid stool, colitis-like symptoms, ODS symptoms, or abdominal pain due to intussusception [2, 4]. Our case initially had symptoms suggestive of ODS, followed by fecal incontinence.
The most common cause of ODS is mechanical obstruction from either structural abnormalities (e.g., rectocele and rectal prolapse) or functional abnormalities (e.g., pelvic dyssynergia). A huge pedunculated polyp may cause persistent internal recto-rectal intussusception presenting as rectal prolapse, especially during bearing down, which could be the mechanical precursor to ODS [6, 7]. Besides intussusception, a huge polyp can also lead to luminal obstruction and overdistension of the rectum. Chronic distension of the rectum leads to hyposensitivity followed by paradoxical rectal contraction, leading to overflow incontinence, which is the seepage type with a sensation of incomplete evacuation requiring frequent toilet visits [7]. These symptoms are similar to those in our case upon presentation, which resolved immediately after resection. The Jorge-Wexner incontinence score used to assess the patientŌĆÖs incontinence showed a marked reduction after the resection.
In our case, an analysis of the biopsy specimen initially reported SRUS; however, the diagnosis was subsequently modified to JP after the final excision biopsy. SRUS and JPs share inflamed granulation tissue on the polyp as a common feature [8]. As a discriminatory feature, the histopathological examination of the excised tumor failed to demonstrate the presence of hypertrophied muscularis mucosa with the extension of muscle fibers upwards between the crypts, which is a sensitive marker of SRUS [9]. JPs are described as hamartomas, a malformation of the layers superficial to the muscularis mucosa [10]. In our case, the patientŌĆÖs history, colonoscopy findings, and superficial biopsy results were inadequate to differentiate between SRUS and JP. Therefore, clinicians should always be aware of this differential in younger patients, as these conditions may have different treatment strategies: biofeedback therapy for SRUS and resection for JPs.
Even though most papers have described the risks of malignant transformation in JPs as almost negligible, there have been reported cases of malignant transformation in younger children [1, 3, 4]. In addition, there is no doubt that juvenile polyposis syndrome is a premalignant condition conferring a higher risk of developing colorectal carcinoma than the general population, as about 50% of juvenile polyposis syndrome patients were reported to harbor adenomatous changes, predominantly low-grade dysplasia [4, 11].
JP (nonpolyposis) was considered a benign hamartoma with an adenomatous change rate of 5.6% to 12% to either focal or lowgrade dysplasia [4]. There were also reported cases of adenomatous changes with adenocarcinoma in situ [5]. In our present case, the JP demonstrated features of high-grade dysplasia, necessitating repeated surveillance endoscopy and eventually prompting a plan for transanal resection due to the mass effect and premalignant features. We would like to highlight two rare points of our case: first, JPs are commonly found in the rectosigmoid colon and other colons, but in our case, it occurred in the anorectum; and second, malignant transformation with the presence of high-grade dysplasia is a rare entity in JPs, but was present in our case.
In a nutshell, SRUS and JPs share similar histopathological features on superficial biopsy. SRUS does not harbor a risk of dysplasia, while JP is hamartoma with a substantial risk of malignant transformation. A long-standing benign rectal mass leads to rectal hyposensitivity and paradoxical rectal contraction with a clinical presentation of fecal incontinence.
Giant solitary JPs of the anus is a rare entity. It is challenging to differentiate JPs and SRUS based on a superficial biopsy. Therefore, any symptomatic polypoidal lesion should be excised as a prophylactic measure due to its premalignant potential.
Notes
Fig.┬Ā1.
Retroflexed endoscopy view of the polypoidal mass in the low rectum. (A) White light. (B) Narrow band imaging.
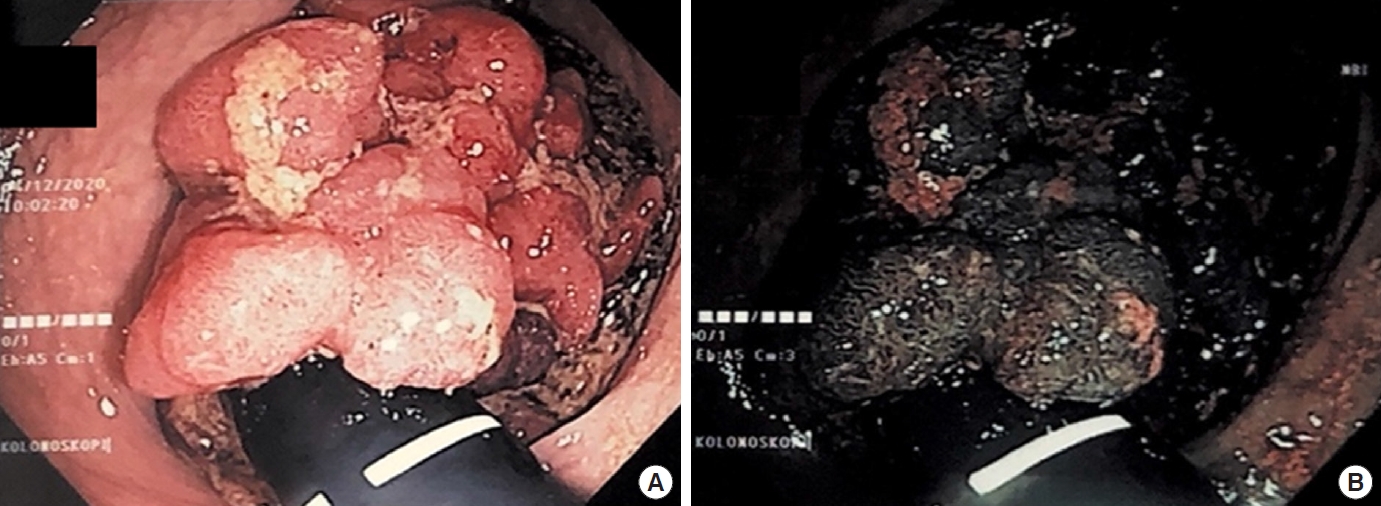
Fig.┬Ā2.
Pelvic magnetic resonance imaging showing a lobulated mass (red arrow) with a long stalk (blue arrows) protruding into the rectum, compressing the bladder anteriorly.

Fig.┬Ā3.
Clinical images. (A) Polypoidal mass protruding from the anal canal. (B) The excised specimen.
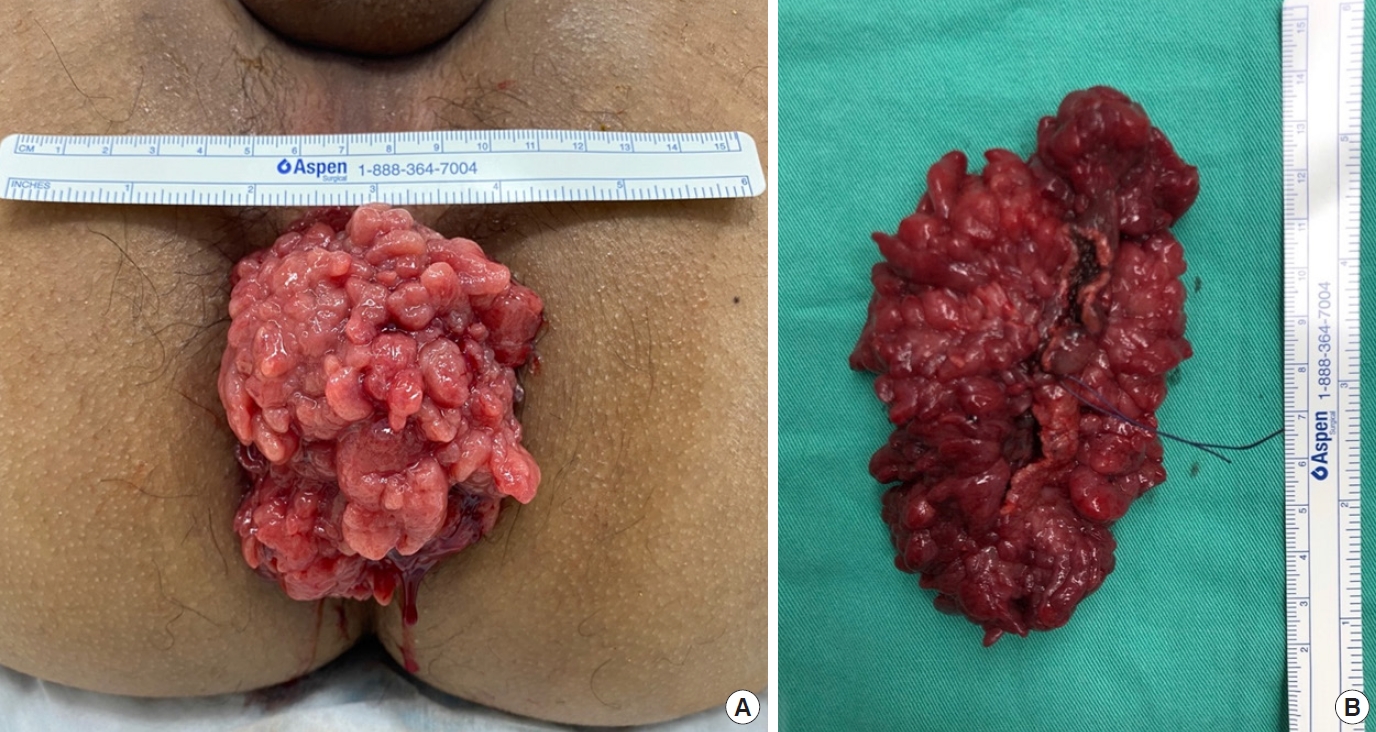
Fig.┬Ā4.
A fragment of colonic tissue harbouring scattered randomly arranged glands exhibiting regenerative atypia. The surrounding stroma is fibrosed, with lymphoplasma cells infiltrates visible. Additionally, the glands are surrounded by strands of hyperplastic smooth muscle fibres. There was no evidence of significant dysplasia. This case was diagnosed as solitary rectal ulcer syndrome (hematoxylin-eosin, ├Ś200).
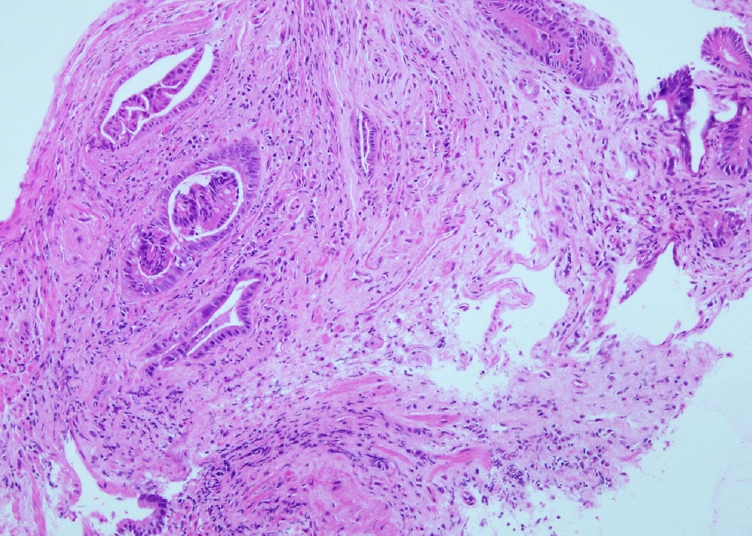
Fig.┬Ā5.
Polypoid colonic tissue composed of proliferation of glands which appear cystically dilated and distorted. The glands are predominantly lined by low-grade dysplastic epithelium. In a few foci, the glands are cribriform and lined with a high-grade dysplastic epithelium and contain necrotic debris (inset image). Additionally, cystitis and crypt abscess are noted. The lamina propria is oedematous and contain inflammatory cells. No features of malignancy identified. The final diagnosis is juvenile polyps with high-grade dysplasia (hematoxylin-eosin, ├Ś40; inset image: ├Ś100).
REFERENCES
1. Ibrahimi N, Septer SS, Lee BR, Garola R, Shah R, Attard TM. Polyp characteristics of nonsyndromic and potentially syndromic juvenile polyps: a retrospective cohort analysis. J Pediatr Gastroenterol Nutr 2019;69:668ŌĆō72.



2. Kay M, Eng K, Wyllie R. Colonic polyps and polyposis syndromes in pediatric patients. Curr Opin Pediatr 2015;27:634ŌĆō41.


3. Hood B, Bigler S, Bishop P, Liu H, Ahmad N, Renault M, et al. Juvenile polyps and juvenile polyp syndromes in children: a clinical and endoscopic survey. Clin Pediatr (Phila) 2011;50:910ŌĆō5.



4. Poddar U, Thapa BR, Vaiphei K, Singh K. Colonic polyps: experience of 236 Indian children. Am J Gastroenterol 1998;93:619ŌĆō22.


5. Gupta SK, Fitzgerald JF, Croffie JM, Chong SK, Pfefferkorn MC, Davis MM, et al. Experience with juvenile polyps in North American children: the need for pancolonoscopy. Am J Gastroenterol 2001;96:1695ŌĆō7.


6. Andromanakos N, Skandalakis P, Troupis T, Filippou D. Constipation of anorectal outlet obstruction: pathophysiology, evaluation and management. J Gastroenterol Hepatol 2006;21:638ŌĆō46.


7. Linardoutsos D. Assessment and treatment of obstructed defecation syndrome. In: Camilleri-Brennan J, editor. Current topics in faecal incontinence. IntechOpen; 2020.

8. Singh B, Mortensen NJ, Warren BF. Histopathological mimicry in mucosal prolapse. Histopathology 2007;50:97ŌĆō102.


9. Zhu QC, Shen RR, Qin HL, Wang Y. Solitary rectal ulcer syndrome: clinical features, pathophysiology, diagnosis and treatment strategies. World J Gastroenterol 2014;20:738ŌĆō44.



- TOOLS








