- Search
| Ann Coloproctol > Volume 39(4); 2023 > Article |
|
Abstract
Purpose
Transanal total mesorectal excision (TaTME) has been proposed to overcome surgical difficulties encountered during rectal resection, especially for patients having high body mass index or low rectal cancer. The aim of this study was to evaluate oncologic outcomes following TaTME.
Methods
This retrospective study included all consecutive patients with rectal cancer who had a TaTME from 2013 to 2019. The main outcome was the incidence of locoregional recurrence by the end of the follow-up period.
Results
Among a total of 81 patients, 96.3% were male, and their mean age was 63ôÝ9 years. The mean body mass index was 30.3ôÝ5.7 kg/m2, and the median distance from tumor to anal verge was 5.0 cm (interquartile range [IQR], 4.0ã6.0 cm). Most patients had a low anterior resection performed (n=80, 98.8%) with a diverting ileostomy (n=64, 79.0%). Distal and circumferential resection margins were positive in 2.5% and 6.2% of patients, respectively. Total mesorectal excision was complete or near complete in 95.1% of patients. A successful resection was achieved in 72 patients (88.9%). After a median follow-up of 27.5 months (IQR, 16.7ã48.1 months), 4 patients (4.9%) experienced locoregional recurrence. Anastomotic leaks were observed in 21 patients (25.9%). At the end of the follow-up, 69 patients (85.2%) were stoma-free.
Conclusion
TaTME was associated with acceptable oncological outcomes, including low locoregional recurrence rates in selected patients with low rectal cancer. Although associated with a high incidence of postoperative morbidities, the use of TaTME enabled a high rate of successful sphincter-saving procedures in selected patients who posed a technical challenge.
For patients with rectal cancer amenable to curative treatment, total mesorectal excision (TME) is the established standard of care and is associated with lower local recurrence rates and improved survival compared with a blunt dissection [1, 2]. Laparoscopic rectal cancer resection is associated with faster recovery of bowel function and shorter hospital stay as compared with open resection without affecting oncological outcomes [3]. However, laparoscopic surgery is associated with technical challenges related to pelvic dissection and the use of laparoscopic staplers within restricted angulations, especially for patients exhibiting high body mass index (BMI), low rectal cancer, or narrow pelvis [4ã8]. To overcome these difficulties, Sylla and colleagues demonstrated the feasibility of transanal TME (TaTME) in 2010 [9]. With this transanal approach, distal mesorectal dissection and stapler placement are potentially easier due to improved exposure [4, 7, 10].
A recent systematic review and meta-analysis by Aubert et al. [11] that compared laparoscopic versus transanal approaches found no differences in local recurrence or standard indicators of acceptable oncologic outcomes (e.g., complete or near-complete resection, negative margins, and harvested lymph nodes). Even though the surgical and oncological results initially observed with TaTME were acceptable as compared with other surgical approaches, recent studies have raised some concerns of high local recurrence rates following TaTME and of a prolonged surgeonsã learning curve required to adequately perform this novel procedure [5, 12ã17]. Further evidence is needed to better define the role of TaTME in rectal cancer management. Therefore, the aim of our study was to assess perioperative and oncologic outcomes following TaTME at a high-volume, tertiary-care colorectal surgery center.
The approval for the study protocol was waived by the Institutional Review Board of the CHU de Quûˋbec - Universitûˋ Laval, and the requirement for informed consent was waived due to the retrospective nature of the analysis.
All patients who had an elective TaTME for rectal cancer from December 2013, when surgeons began performing this technique at our center, to December 2019 were included in this retrospective study. No restriction was applied for clinical tumor stage or for history of pelvic cancer, surgery, or radiation. Patients whose laparoscopic surgery could represent a potential surgical challenge (high BMI, narrow pelvis, distal lesion, male sex, etc.) were selected for a transanal approach in multidisciplinary tumor boards.
All TaTME were performed by 4 fellowship-trained colorectal surgeons with significant experience in laparoscopic surgery and transanal endoscopic surgery. A team of 2 surgeons performed each surgery via sequential transanal and abdominal dissection. All patients received a preoperative mechanical bowel preparation. After the insertion of a transanal endoscopic microsurgery (TEM) proctoscope or transanal minimally invasive surgery platform, pneumorectum was created. A purse-string suture was occasionally placed to close the rectal stump distal to the rectal tumor for higher rectal lesions. For very low intersphincteric dissections, a suture was not used to avoid damaging the distal margin, and a gauze was inserted into the stump to prevent spillage. This was followed by a full-thickness transection of the rectal wall and a cephalad transanal mesorectal dissection. The specimen was extracted through a Pfannenstiel incision or a left lower quadrant transverse incision. The anastomosis was either stapled or handsewn, based on the surgeonãs preference. When a delayed coloanal anastomosis was created, a pull-through technique was used with the distal rectum being pulled through the anus and fixed to the anal verge with 1 or 2 interrupted sutures. Approximately 1 week after the primary surgery, the rectal stump was excised at the anal verge and was then anastomosed using interrupted full-thickness absorbable sutures [18]. A laparoscopic transabdominal mobilization technique was performed in a similar fashion as during laparoscopic lower anterior resection.
Patients had a standard oncological follow-up, with postoperative computed tomography (CT) scans every 6 to 12 months for the first 3 years than every 12 months for the next 2 years. Water soluble enema was performed systematically before stoma closure to rule out anastomotic leak.
To ensure the evaluation of all consecutive patients since 2013, the archive code attributed to a rectal resection was used to query our clinical database. Operative protocols were then retrieved from the hospital data system and were hand searched to determine the surgical approach employed for each patient. For eligible patients, demographic data at the time of surgery, perioperative evolution and clinical information from postoperative follow-up were obtained through a retrospective chart review from our data system through March 2021. Radiological reports of CT scans, magnetic resonance imaging studies, and positron emission tomography (PET) scans performed either at our center or at the patientãs local medical center were considered as radiological evaluation. The original histopathological reports were considered for the acquisition of oncological data.
The primary outcome was the incidence of locoregional recurrence during the follow-up period. It was defined either as a mass that increased in size on subsequent imaging studies or as a malignant lesion confirmed by a pathologic report following a biopsy or a surgery. Secondary outcomes were the incidence of multifocal and distant recurrence. A multifocal local recurrence was defined as more than one lesion identified in the pelvic area in imaging studies or in a pathological report. A metachronous tumor outside the pelvis that was confirmed either radiologically or pathologically was considered a distant metastasis.
Other secondary outcomes were the quality of the surgical specimen (complete, nearly complete, or incomplete [19]), the incidence of positive distal and circumferential resection margins (CRMs) (both defined as the presence of adenocarcinoma at ãÊ1 mm), and the number of positive lymph nodes and total lymph nodes dissected. A composite outcome described in the ACOSOG Z6051 Randomized Clinical Trial was also used as a secondary outcome to evaluate oncological completeness [20]. In this article, a successful resection was defined as meeting all 3 of the following criteria: a negative distal resection margin (>1 mm), a negative CRM (>1 mm), and a complete or nearly complete TME. Perioperative blood loss, operative time, and length of stay were also assessed. The incidence of postoperative complications (classified according to the Clavien-Dindo [CD] classification system [21]), reoperations, rehospitalizations, and mortality were evaluated at postoperative day 30. The incidence of anastomotic complications (leak, bleeding, or stenosis) was assessed during the entire follow-up period. Anastomotic leak was defined as either clinical, endoscopic, or radiological evidence of an intestinal wall defect resulting in communication with the extraluminal compartments [22]. Finally, the status of the stoma at the end of the follow-up period was assessed.
For demographic features and outcomes, continuous data were presented as mean and standard deviation with significance analyzed using a t-test procedure, or as median and interquartile range (IQR) with significance analyzed using a Wilcoxon 2-sample test depending on the normality of the data distribution. Categorical data were presented in proportion with significance analyzed using a Fisher exact test.
For the outcome of anastomotic leak, variables with a P-value of ãÊ0.05 in univariable analysis were included in a multivariable logistic regression analysis. For these potential risk factors, odds ratios were produced. A P-value of ãÊ0.05 was considered significant. Statistical analyses were performed using SAS University edition (SAS Institute Inc).
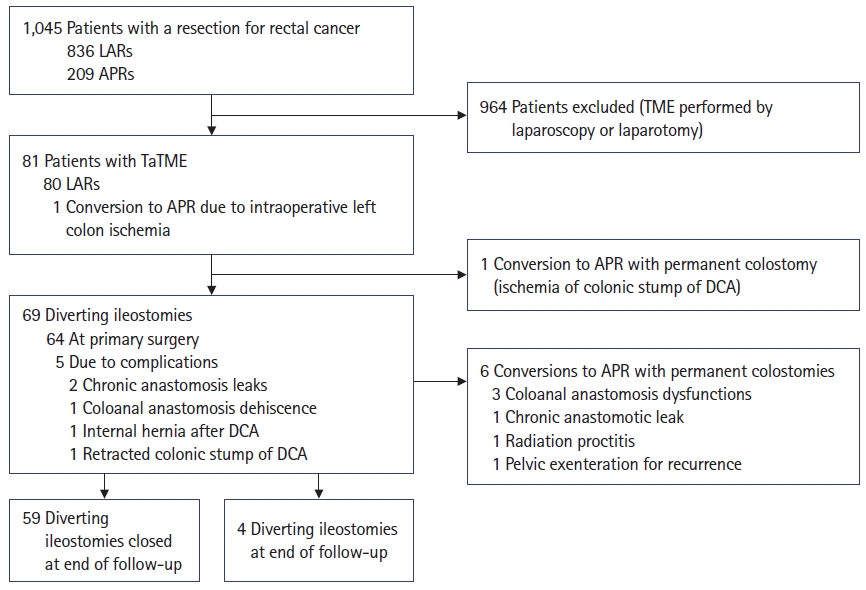
From December 2013 to December 2019, 1,045 patients underwent resection of rectal cancer at our center; 81 of the patients (7.8%) had a TaTME (Fig. 1). In this cohort of patients, 96.3% were male, and their mean age was 63ôÝ9 years. Mean BMI was 30.3ôÝ5.7 kg/m2, and 39 patients (48.1%) were considered obese (BMI, ãË30.0 kg/m2) (Table 1). Clinical evaluations suggested that most patients had a cT3 tumor (59.5%), and lymph node invasion was suspected from preoperative imaging studies in 37 patients (46.8%). The most frequent indication noted for choosing a transanal approach for TME was a distal rectal lesion (n=65, 80.2%), with a median distance from the tumor to the anal margin of 5.0 cm (IQR, 4.0ã6.0 cm). In this cohort, 59.3% of patients received neoadjuvant radiochemotherapy and 11.1% of patients received neoadjuvant radiotherapy only.
A single patient had a planned laparotomy due to a recurrence after a lower anterior resection that was complicated by an anastomotic leak (Table 2). No conversions to laparotomy were observed in this cohort. One patient had an abdominoperineal resection due to intraoperative left colon ischemia caused insufficient colonic length for coloanal anastomosis. A TEM platform was used to perform the procedure in most patients (71.6%), and a diverting ileostomy was created initially in 64 patients (79.0%). A majority of anastomoses created were primary handsewn coloanal anastomosis (65.0%), with a delayed coloanal anastomosis (DCA) being performed in 18 patients (22.5%). The median operative time was 300 minutes (IQR, 262ã360 minutes).
In this cohort of patients with diagnosis of rectal cancer, the median distal margin was 15.0 mm (IQR, 8.0ã25.0 mm), and distal margins were positive in 2 patients (2%) patients (Table 3). The median CRM was 8.0 mm (IQR, 5.0ã13.0 mm), and 5 patients (6.2%) had a positive CRM. TME was complete or near complete in 95.1% of patients, and a median of 25 (IQR, 18ã29) lymph nodes were harvested per patient, which revealed that 18.5% of patients had lymph node invasion. A successful resection as defined by the composite outcome was achieved in 72 patients (88.9%). At least 1 year of postoperative follow-up was available for 74 of 81 patients (91.4%).
After a median postoperative follow-up of 27.5 months (IQR, 16.7ã48.1 months), locoregional recurrences were observed in 4 patients (4.9%), where of which 3 (3.7%) had multifocal local recurrences. The first patient (patient 1) with locoregional recurrence was an 80-year-old male who had a transanal approach for rectal cancer recurrence (Table 4). During the primary surgery, a tumor implant near the left ureter was resected. A new onset of left hydronephrosis was observed on postoperative radiological follow-up, with a 2-cm lesion observed at the transition point near the site of the previously resected implant. The management is unknown, as the patient was followed in his regional medical center. The second patient (patient 5) was a 51-year-old male who had a recurrence invading the prostate, right ureter, and bladder with a pelvic nodal involvement (Table 4). He had a pelvic exenteration with adjuvant chemoradiotherapy. The third patient (patient 7) was a 52-year-old male with an anastomotic recurrence, left pelvic nodal involvement, suspected peritoneal carcinomatosis, and multiple right pulmonary metastases diagnosed on postoperative PET-scan, who had a palliative chemotherapy (Table 4). The last patient (patient 9) with locoregional recurrence was a 56-year-old male with right pararectal recurrence, sacrum involvement, paraaortic and pelvic lymph node metastases, with multiple hepatic metastases. He received palliative chemoradiotherapy (Table 4). Globally, tumor recurrence was observed in 13 patients (16.0%), with 11 patients with distant metastases: 5 patients had pulmonary metastases, 4 had hepatic metastases, and 2 were diagnosed with both pulmonary and hepatic metastases of rectal adenocarcinomas (Tables 3, 4). Median time from primary surgery to recurrence was 17.3 months (IQR, 9.9ã25.9 months).
After TaTME, median length of hospital stay was 4 days (IQR, 3ã8 days), and 70.4% of patients had only minor complications or no complications in the first 30 postoperative days (Table 5). Major postoperative complications (CD grade of ãËIII) occurred in 29.6%. Reoperation was required in 20 patients (24.7%), and rehospitalization was necessary in 13 patients (16.0%). No urethral injury occurred in this cohort of patients. Internal hernias were observed in 5 patients (6.2%), with the small bowel passing under the mesentery of the left colon. All but 1 of these patients had a DCA at the initial surgery. No mortality was observed 30 days postoperatively.
Anastomotic leaks were observed in 21 of 80 patients (26.3%). When the first 20 patients were compared with the last 20 patients, no significant difference was observed in the frequency of an anastomotic leak (9 patients with leak in the first 20 [45.0%] vs. 4 patients with leak in the last 20 [20.0%], P=0.176). However, primary coloanal anastomosis was associated with fewer anastomotic leaks than DCA (21.0% [13 of 62] vs. 44.4% [8 of 18], P=0.067). When only primary coloanal anastomoses were considered, handsewn anastomoses were associated with fewer anastomotic leaks as compared with stapled anastomoses (15.4% [8 of 52] vs. 50.0% [5 of 10], P=0.027). In univariable analyses, a statistically significant correlation was observed for the type of anastomosis (P=0.010), favoring a primary handsewn coloanal anastomosis instead of a stapled anastomosis or DCA (Table 6). Estimated blood loss also showed a statistically significant correlation with anastomotic leak in the univariable analysis (P=0.031). However, both variables did not reach statistical significance in multivariable analysis (Table 7).
Transanal drainage under general anesthesia was required for 14 of the 21 patients (66.7%) to treat the anastomotic leak initially (Table 5). By the end of the study follow-up period, stoma had been created in 5 patients who experienced an anastomotic leak, 3 by end colostomy after abdominoperineal resection and 2 by diverting ileostomy. There were 9 patients (11.1%) who required either dilations under general anesthesia or bougie dilators during a colonoscopy exam to treat anastomotic stenosis.
During the follow-up period, diverting ileostomies were closed a median of 235 days (IQR, 189.5ã312.0 days) after primary surgery. At the end of the follow-up period, 69 patients (85.2%) were stoma-free, 8 (9.9%) had an end colostomy, and 4 (4.9%) still had a diverting ileostomy (Fig. 1).
In this retrospective study examining oncologic outcomes of patients following TaTME, the risk of locoregional recurrence was low (4.9%) after a median postoperative follow-up of 2 years, with 3.7% of multifocal local recurrences. A relatively high risk of anastomotic leak was observed in this cohort, but most patients were stoma free at the end of the follow-up period.
The risk of locoregional recurrence of 4.9% observed in this retrospective study is comparable with some previous studies assessing oncological outcomes after TaTME. Recurrence was observed in 2.0% to 7.6% of patients assessed in previous studies after postoperative follow-up of 15 to 36 months [14, 23ã28]. One technical aspect that may have contributed to our outcomes was the decision to systematically perform the transanal dissection in pairs of colorectal surgeons. We did this to increase surgeon experience and allow concerted decision-making on dissection plans. This partnering may have contributed to the high rate of complete or near-complete TME observed in this cohort, which is comparable with rates in the literature for TaTME, typically 89% to 100% [17, 23, 24, 26ã33]. The high rate of successful resection observed in this cohort is also comparable with the results of previous studies using the same composite outcome for open, laparoscopic or transanal rectal resection, with successful rate ranging from 71% to 86.9% [20, 34]. Because completion of TME is correlated with lower locoregional recurrence rates, this may partially explain our oncologic results, namely recurrence rates after TaTME similar to those seen after laparoscopic TME despite using TaTME for more complex resections [1, 2].
Another contributing factor to low recurrence rates and satisfactory oncologic outcomes was the high-volume of TaTME performed at our center, with 74 TaTMEs performed over the last 4 years. A systematic review with meta-analysis by Deijen et al. [35] showed a clear trend toward less locoregional recurrence when TaTME was performed at a center with more than 30 total cases completed. A consensus published by Penna et al. [36] in 2016 recommended a mean of 14 cases per year per center required to maintain competences to performed TaTME. With 19 cases per year in the last 4 years, our study further demonstrates the potential benefits of concentrating certain surgical techniques at specialty centers to optimize the quality of treatment.
When compared with previous studies on TaTME, the risk of postoperative complications was significantly higher in our cohort of patients. Indeed, morbidities were observed in 53.1% of our patients, with 29.6% classified as CD grade of ãËIII. Some previous reports demonstrated postoperative complications in 24.5% to 52.2% of patients, with 10% to 24.5% categorized as CD grade of ãËIII [17, 23, 24, 26ã30, 32, 35, 37]. It appears that the higher rate of complications we observed had little-to-no impact on the typical postoperative course, however, as the median length of stay (4 days) observed in our cohort was comparable with previous studies (4ã8 days) [17, 23, 24, 28ã30, 32, 33, 35, 37]. Anastomotic leak was a postoperative complication in 25.9% of the cohort, which is higher than the incidence of leak reported for previous studies (5.0%ã17.3%), and may have significantly contributed to the overall higher rate of postoperative comorbidities that we observed [14, 16, 23, 24, 26ã29, 32, 33, 35, 37]. The definition that we used for an anastomotic leak, however, may have contributed to the high risk observed in the study. Indeed, some previous studies considered only early leaks 30 days postsurgery or leaks requiring reoperation, whereas we considered anastomotic leaks occurring during the entire follow-up period regardless of whether treatment was required [14, 17, 23, 25, 27].
Furthermore, the choice of anastomosis technique when we first introduced the procedure at our institution could have also influenced our overall incidence of leaks in the study. Indeed, stapled coloanal anastomosis or DCA, which were used more often when we first began performing TaTME, were associated with more anastomotic leaks as compared with primary handsewn coloanal anastomosis. This latter anastomosis technique was used in 19 of our last 20 patients, and anastomotic leaks were observed in only 20.0% (4 of 20) of these patients. Handsewn anastomoses are often more appropriate for very low coloanal anastomosis due to inadequate stump length for a purse-string suture, which partially explains our gradual change of practice [4]. Thus, the choice of anastomosis could have contributed to the learning curve we experienced as the incidence of anastomotic leak was higher in the early phase of the study.
The high risk of anastomotic leak may also be explained by our local practice choices for TaTME with regards to patient selection and type of surgery. Because operative time is often longer for TaTME, as compared with laparoscopic TME, when transanal and abdominal dissection are not performed simultaneously, we favored patients who were more likely to benefit from a transanal dissection when offering the procedure. This is evidenced by the small proportion of rectal cancers, only 7.8% of patients, treated with a transanal dissection at our center during the study period, which is low when compared with 20% approached by a transanal dissection in a recent international audit [14]. Since laparoscopic TME with coloanal anastomosis is more difficult in male patients with low rectal cancer and a high BMI, patients with these characteristics were selected predominantly for a transanal approach in our cohort [6ã8]. Indeed, both our proportion of male patients (96.3% vs. 60%ã80%) and the mean BMI of our patients (30.3 kg/m2 vs. 25.2ã29.8 kg/m2) were higher than in some previous reports [14, 16, 17, 23, 24, 26ã33, 35, 37]. However, male patients with low rectal cancer and high BMI also have an increased risk of anastomotic leak after either laparoscopic TME or TaTME, which could have contributed to our results [32, 38, 39].
As for our local practice choices for the type of surgery, we planned a coloanal anastomosis preoperatively in all of our patients to favor preservation of intestinal continuity, despite the previously mentioned risk factors for anastomotic leak. Indeed, our rate of anastomosis, either primary or delayed, was high compared with some previous studies (98.8% vs. 70%ã91%) [14, 16, 17, 24, 26ã29, 32, 33, 35, 37]. Even though end colostomies were ultimately required for 9 patients for various indications, 85.2% of patients were free of stoma at the end of the follow-up period. This proportion of stoma-free patients is higher than some previous studies, which reported 52% to 69% of patients free of stoma at the end of follow-up [14, 24, 27]. Although our risk of anastomotic leak was significantly higher than previous reports on TaTME, this cohort of patients had an overall favorable postsurgical evolution, with a high rate of successful restoration of bowel continuity.
A potential limitation is the retrospective nature of our cohort, with resulting information bias. However, perioperative and follow-up data were well documented for most patients in our data system, and surgical indications for a transanal approach were reviewed by each operating surgeon to ensure adequate documentation of the decision process. Due to this retrospective design, patient selection process was not standardized. This resulted in a selection bias in which patients were selected for a transanal approach based on the morphological features representing potentially more complex laparoscopic resections. Also, due to our monocentric study design, the size of our cohort compared to larger multicenter series is a potential limitation, as it resulted in a small number of locoregional recurrences, which prevented the realization of statistical analyses for potential risk factors for this outcome. The absence of a control group could also be potential limitations of our study. Additionally, because our center is a tertiary center for colorectal surgery, some patientsã postoperative follow-up was assured by surgeons at regional hospitals. Even though we had access to many imaging studies performed outside of our medical center, clinical and endoscopic follow-ups were not always available. This may have led to a loss of some follow-up data, and possibly to an underestimation of recurrence rates. Results of ongoing randomized clinical trials comparing laparoscopic TME with TaTME will eventually contribute to a better understanding of this problem [40, 41].
In our study, the use of TaTME was associated with acceptable oncological outcomes, including low locoregional recurrence rates in selected patients with low rectal cancer. Although associated with a high incidence of postoperative morbidities, the use of TaTME enabled a high rate of successful sphincter-saving procedures in this cohort of selected patients who posed a technical challenge.
Fig.ô 1.
Flowchart detailing patients evaluated and included in the study. LAR, lower anterior resection; APR, abdominoperineal resection; TME, total mesorectal excision; TaTME, transanal total mesorectal excision; DCA, delayed coloanal anastomosis.
Tableô 1.
Patient demographics
| Demographic | Value (n=81) |
|---|---|
| Age (yr) | 63ôÝ9 |
| BMI (kg/m2) | 30.3ôÝ5.7 |
| ãNormal weight (<25.0) | 11 (13.6) |
| ãOverweight (ãË25.0, <30.0) | 31 (38.3) |
| ãObesity class I (ãË30.0, <35.0) | 23 (28.4) |
| ãObesity class II (ãË35.0, <40.0) | 10 (12.3) |
| ãObesity class III (ãË40) | 6 (7.4) |
| Sex | |
| ãMale | 78 (96.3) |
| ãFemale | 3 (3.7) |
| Charlson score | 4 (3ã5) |
| Preoperative histology on biopsy | |
| ãAdenocarcinoma | 79 (97.5) |
| ãAdenoma | 2 (2.5) |
| Clinical tumor stagea | |
| ãcT1 | 4 (5.1) |
| ãcT2 | 24 (30.4) |
| ãcT3 | 47 (59.5) |
| ãcT4 | 2 (2.5) |
| ãUnavailable | 2 (2.5) |
| Positive nodal statusa | 37 (46.8) |
| Distance from anal verge (cm) | 5 (4ã6) |
| ãLow rectum (ãÊ5) | 45 (55.6) |
| ãMid rectum (>5 and ãÊ10) | 34 (42.0) |
| ãHigh rectum (>10) | 1 (1.2) |
| Neoadjuvant treatment | |
| ãNeoadjuvant radiochemotherapy | 48 (59.3) |
| ãNeoadjuvant radiotherapy only | 9 (11.1) |
| ãNone | 24 (29.6) |
| Indication for transanal approachb | |
| ãDistal lesions | 65 (80.2) |
| ãBMI | 34 (42.0) |
| ãNarrow pelvis | 7 (8.6) |
| ãPost-TEM | 5 (6.2) |
| ãRedo surgery | 4 (4.9) |
| ãRecurrence | 3 (3.7) |
| ãGiant rectal villous adenoma | 1 (1.2) |
| ãProstatomegaly | 1 (1.2) |
Tableô 2.
Characteristics of the primary surgery (n=81)
| Characteristic | Value |
|---|---|
| Surgical approach | |
| ãLaparoscopic | 80 (98.8) |
| ãOpen | 1 (1.2) |
| ãConversion to laparotomy | 0 (0) |
| Surgical platform | |
| ãTransanal endoscopic microsurgery | 58 (71.6) |
| ãTransanal minimally invasive surgery | 23 (28.4) |
| Type of resection | |
| ãLower anterior resection | 80 (98.8) |
| ãAbdominoperineal resection | 1 (1.2) |
| Surgical drain | 18 (22.2) |
| Stoma at primary surgery | |
| ãDiverting ileostomy | 64 (79.0) |
| ãNo stoma | 16 (19.8) |
| ãPermanent colostomy | 1 (1.2) |
| Anastomosis technique (n=80)a | |
| ãPrimary handsewn CAA | 52 (65.0) |
| ãPrimary stapled CAA | 10 (12.5) |
| ãDelayed coloanal anastomosis | 18 (22.5) |
| Operative time (min) | 300 (262ã360) |
| Blood loss (mL) | 100 (30ã200) |
Tableô 3.
Tumor pathology and oncologic outcomes (n=81)
| Variable | Value |
|---|---|
| Pathological diagnosis | |
| ãRectal adenocarcinoma | 70 (86.4) |
| ãAbsence of residual tumor | 10 (12.3) |
| ãEpidermoid carcinoma | 1 (1.2) |
| Pathological tumor stage | |
| ãpT0 | 11 (13.6) |
| ãpT1 | 12 (14.8) |
| ãpT2 | 27 (33.3) |
| ãpT3 | 31 (38.3) |
| Pathological nodal stage | |
| ãpN0 | 61 (75.3) |
| ãpN1 | 16 (19.8) |
| ãpN2 | 4 (4.9) |
| Largest tumor dimension (cm) | 2.0 (1.5ã3.5) |
| Margin | |
| ãDistal margin (mm) | 15 (8ã25) |
| ãPositive distal margin | 2 (2.5) |
| ãCircumferential margin (mm) | 8 (5ã13) |
| ãPositive circumferential margin | 5 (6.2) |
| Quality of TME | |
| ãComplete | 64 (79.0) |
| ãNear complete | 13 (16.0) |
| ãIncomplete | 4 (4.9) |
| Composite outcomea | 72 (88.9) |
| Invasion | |
| ãPerinervous | 13 (16.0) |
| ãLymphatic | 14 (17.3) |
| ãVeinous | 17 (21.0) |
| Tumor deposit | 7 (8.6) |
| Tumor perforation | 1 (1.2) |
| No. of LNs harvested | 25 (18ã29) |
| Positive LN | 15 (18.5) |
| Adjuvant chemotherapy | 30 (37.0) |
| Adjuvant radiotherapy | 1 (1.2) |
| Recurrence | 13 (16.0) |
| ãLocoregional recurrenceb | 4 (4.9) |
| ãDistant recurrence | 11 (13.6) |
Tableô 4.
Demographic features and oncologic characteristics of patients with rectal cancer recurrence
BMI, body mass index; pTN, pathologic assessment of the primary tumor and lymph node status; CRM, circumferential resection margin; TME, total mesorectal excision; CRT, chemoradiotherapy; CT, chemotherapy; LR, locoregional recurrence; DM, distant metastasis; MR, multifocal local recurrence; RT, radiotherapy.
Tableô 5.
Complications of the primary surgery (n=81)
| Variable | Value |
|---|---|
| Length of stay (day) | 4 (3ã8) |
| Complication classificationa | |
| ãNone | 38 (46.9) |
| ãI | 18 (22.2) |
| ãII | 1 (1.2) |
| ãIIIa | 4 (4.9) |
| ãIIIb | 18 (22.2) |
| ãIVa | 2 (2.5) |
| ãIVb | 0 (0) |
| Anastomotic leak (n=80)b | 21 (26.3) |
| ããÊ30 day | 15 (18.8) |
| ã>30 day | 6 (7.5) |
| Treatments needed for leakc | |
| ãTransrectal drainage under general anesthesia | 14 (66.7) |
| ãLaparoscopic surgery | 5 (23.8) |
| ãPercutaneous drainage | 2 (9.5) |
| ãEndoscopic drainage | 1 (4.8) |
| ãConservative management | 1 (4.8) |
| ãLaparotomy | 0 (0) |
| Anastomosis bleeding (n=80)b | 0 (0) |
| Anastomosis stenosis (n=80)b | 9 (11.1) |
| Ileusd | 10 (12.3) |
| Small bowel obstructiond | 11 (13.6) |
| ãStoma site | 6 (7.4) |
| ãInternal hernia | 5 (6.2) |
| Reoperationd | 20 (24.7) |
| Rehospitalizationd | 13 (16.0) |
Tableô 6.
Analysis of ALs during follow-up (n=80)a
Tableô 7.
Anastomotic leaks during follow-up using multivariable logistic regression analysis (n=80)a
REFERENCES
1. Knol J, Keller DS. Total mesorectal excision technique: past, present, and future. Clin Colon Rectal Surg 2020;33:134ã43.



2. Heald RJ, Husband EM, Ryall RD. The mesorectum in rectal cancer surgery: the clue to pelvic recurrence? Br J Surg 1982;69:613ã6.



3. van der Pas MH, Haglind E, Cuesta MA, Fû¥rst A, Lacy AM, Hop WC, et al. Laparoscopic versus open surgery for rectal cancer (COLOR II): short-term outcomes of a randomised, phase 3 trial. Lancet Oncol 2013;14:210ã8.


4. Penna M, Knol JJ, Tuynman JB, Tekkis PP, Mortensen NJ, Hompes R. Four anastomotic techniques following transanal total mesorectal excision (TaTME). Tech Coloproctol 2016;20:185ã91.




5. 2017 European Society of Coloproctology (ESCP) collaborating group. An international multicentre prospective audit of elective rectal cancer surgery; operative approach versus outcome, including transanal total mesorectal excision (TaTME). Colorectal Dis 2018;20 Suppl 6:33ã46.



6. Akiyoshi T, Kuroyanagi H, Oya M, Konishi T, Fukuda M, Fujimoto Y, et al. Factors affecting the difficulty of laparoscopic total mesorectal excision with double stapling technique anastomosis for low rectal cancer. Surgery 2009;146:483ã9.


7. Penna M, Cunningham C, Hompes R. Transanal total mesorectal excision: why, when, and how. Clin Colon Rectal Surg 2017;30:339ã45.



8. Adamina M, Buchs NC, Penna M, Hompes R, St.Gallen Colorectal Consensus Expert Group. St.Gallen consensus on safe implementation of transanal total mesorectal excision. Surg Endosc 2018;32:1091ã103.



9. Sylla P, Rattner DW, Delgado S, Lacy AM. NOTES transanal rectal cancer resection using transanal endoscopic microsurgery and laparoscopic assistance. Surg Endosc 2010;24:1205ã10.



10. FernûÀndez-Hevia M, Delgado S, Castells A, Tasende M, Momblan D, DûÙaz del Gobbo G, et al. Transanal total mesorectal excision in rectal cancer: short-term outcomes in comparison with laparoscopic surgery. Ann Surg 2015;261:221ã7.


11. Aubert M, Mege D, Panis Y. Total mesorectal excision for low and middle rectal cancer: laparoscopic versus transanal approach: a meta-analysis. Surg Endosc 2020;34:3908ã19.



12. Ma B, Gao P, Song Y, Zhang C, Zhang C, Wang L, et al. Transanal total mesorectal excision (taTME) for rectal cancer: a systematic review and meta-analysis of oncological and perioperative outcomes compared with laparoscopic total mesorectal excision. BMC Cancer 2016;16:380.




13. Courval V, Drolet S, Bouchard A, Bouchard P. The role of transanal (Ta) dissection in the management of difficult primary and recurrent rectal cancer. BMJ Open Gastroenterol 2019;6:e000305.



14. Wasmuth HH, Faerden AE, Myklebust Tû
, Pfeffer F, Norderval S, Riis R, et al. Transanal total mesorectal excision for rectal cancer has been suspended in Norway. Br J Surg 2020;107:121ã30.



15. Larsen SG, Pfeffer F, Kû¡rner H, Norwegian Colorectal Cancer Group. Norwegian moratorium on transanal total mesorectal excision. Br J Surg 2019;106:1120ã1.



16. Koedam TW, Veltcamp Helbach M, van de Ven PM, Kruyt PM, van Heek NT, Bonjer HJ, et al. Transanal total mesorectal excision for rectal cancer: evaluation of the learning curve. Tech Coloproctol 2018;22:279ã87.



17. Lee L, Kelly J, Nassif GJ, deBeche-Adams TC, Albert MR, Monson JR. Defining the learning curve for transanal total mesorectal excision for rectal adenocarcinoma. Surg Endosc 2020;34:1534ã42.



18. Hallet J, Bouchard A, Drolet S, Milot H, Desrosiers E, Lebrun A, et al. Anastomotic salvage after rectal cancer resection using the Turnbull-Cutait delayed anastomosis. Can J Surg 2014;57:405ã11.



19. Nagtegaal ID, van de Velde CJ, van der Worp E, Kapiteijn E, Quirke P, van Krieken JH, et al. Macroscopic evaluation of rectal cancer resection specimen: clinical significance of the pathologist in quality control. J Clin Oncol 2002;20:1729ã34.


20. Fleshman J, Branda M, Sargent DJ, Boller AM, George V, Abbas M, et al. Effect of laparoscopic-assisted resection vs open resection of stage II or III rectal cancer on pathologic outcomes: the ACOSOG Z6051 randomized clinical trial. JAMA 2015;314:1346ã55.



21. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 2004;240:205ã13.



22. Rahbari NN, Weitz J, Hohenberger W, Heald RJ, Moran B, Ulrich A, et al. Definition and grading of anastomotic leakage following anterior resection of the rectum: a proposal by the International Study Group of Rectal Cancer. Surgery 2010;147:339ã51.


23. Lacy AM, Tasende MM, Delgado S, Fernandez-Hevia M, Jimenez M, De Lacy B, et al. Transanal total mesorectal excision for rectal cancer: outcomes after 140 patients. J Am Coll Surg 2015;221:415ã23.


24. DãAndrea AP, McLemore EC, Bonaccorso A, Cuevas JM, Basam M, Tsay AT, et al. Transanal total mesorectal excision (taTME) for rectal cancer: beyond the learning curve. Surg Endosc 2020;34:4101ã9.



25. van Oostendorp SE, Belgers HJ, Bootsma BT, Hol JC, Belt EJ, Bleeker W, et al. Locoregional recurrences after transanal total mesorectal excision of rectal cancer during implementation. Br J Surg 2020;107:1211ã20.




26. Hol JC, van Oostendorp SE, Tuynman JB, Sietses C. Long-term oncological results after transanal total mesorectal excision for rectal carcinoma. Tech Coloproctol 2019;23:903ã11.




27. Perdawood SK, Kroeigaard J, Eriksen M, Mortensen P. Transanal total mesorectal excision: the Slagelse experience 2013-2019. Surg Endosc 2021;35:826ã36.



28. Gardner IH, Kelley KA, Abdelmoaty WF, Sharata A, Hayman AV, Whiteford MH. Transanal total mesorectal excision outcomes for advanced rectal cancer in a complex surgical population. Surg Endosc 2022;36:167ã75.



29. Veltcamp Helbach M, van Oostendorp SE, Koedam TW, Knol JJ, Stockmann HB, Oosterling SJ, et al. Structured training pathway and proctoring; multicenter results of the implementation of transanal total mesorectal excision (TaTME) in the Netherlands. Surg Endosc 2020;34:192ã201.



30. Veltcamp Helbach M, Deijen CL, Velthuis S, Bonjer HJ, Tuynman JB, Sietses C. Transanal total mesorectal excision for rectal carcinoma: short-term outcomes and experience after 80 cases. Surg Endosc 2016;30:464ã70.



31. Penna M, Hompes R, Arnold S, Wynn G, Austin R, Warusavitarne J, et al. Transanal total mesorectal excision: international registry results of the first 720 cases. Ann Surg 2017;266:111ã7.


32. Penna M, Hompes R, Arnold S, Wynn G, Austin R, Warusavitarne J, et al. Incidence and risk factors for anastomotic failure in 1594 patients treated by transanal total mesorectal excision: results from the International TaTME Registry. Ann Surg 2019;269:700ã11.


33. Buchs NC, Wynn G, Austin R, Penna M, Findlay JM, Bloemendaal AL, et al. A two-centre experience of transanal total mesorectal excision. Colorectal Dis 2016;18:1154ã61.



34. Perdawood SK, Thinggaard BS, Bjoern MX. Effect of transanal total mesorectal excision for rectal cancer: comparison of shortterm outcomes with laparoscopic and open surgeries. Surg Endosc 2018;32:2312ã21.



35. Deijen CL, Tsai A, Koedam TW, Veltcamp Helbach M, Sietses C, Lacy AM, et al. Clinical outcomes and case volume effect of transanal total mesorectal excision for rectal cancer: a systematic review. Tech Coloproctol 2016;20:811ã24.




36. Penna M, Hompes R, Mackenzie H, Carter F, Francis NK. First international training and assessment consensus workshop on transanal total mesorectal excision (taTME). Tech Coloproctol 2016;20:343ã52.



37. Detering R, Roodbeen SX, van Oostendorp SE, Dekker JT, Sietses C, Bemelman WA, et al. Three-year nationwide experience with transanal total mesorectal excision for rectal cancer in the netherlands: a propensity score-matched comparison with conventional laparoscopic total mesorectal excision. J Am Coll Surg 2019;228:235ã44.


38. Rullier E, Laurent C, Garrelon JL, Michel P, Saric J, Parneix M. Risk factors for anastomotic leakage after resection of rectal cancer. Br J Surg 1998;85:355ã8.



39. Qu H, Liu Y, Bi DS. Clinical risk factors for anastomotic leakage after laparoscopic anterior resection for rectal cancer: a systematic review and meta-analysis. Surg Endosc 2015;29:3608ã17.



40. Lelong B, de Chaisemartin C, Meillat H, Cournier S, Boher JM, Genre D, et al. A multicentre randomised controlled trial to evaluate the efficacy, morbidity and functional outcome of endoscopic transanal proctectomy versus laparoscopic proctectomy for low-lying rectal cancer (ETAP-GRECCAR 11 TRIAL): rationale and design. BMC Cancer 2017;17:253.




- TOOLS
-
METRICS

-
- 0 Crossref
- Scopus
- 2,125 View
- 49 Download
- Related articles in ACP
-
Transanal local excision in early rectal cancer: report of 1 case.1992 December;8(3)







