- Search
| Ann Coloproctol > Epub ahead of print |
|
Abstract
Purpose
This study was performed to evaluate the prognostic value of preoperative C-reactive protein to albumin ratio (CAR) in older patients with colorectal cancer (CRC) undergoing curative resection.
Methods
We retrospectively analyzed 244 older patients (aged 75 years or higher) with pathological stage II or III CRC who underwent curative surgery between 2008 and 2016. The optimal value of CAR was calculated and its correlation with the clinicopathological factors and prognosis was examined.
Results
The optimal cutoff value of the CAR was 0.085. High preoperative CAR was significantly associated with high carcinoembryonic antigen levels (P=0.001), larger tumor size (P<0.001), and pT factor (P=0.001). On multivariate analysis, high CAR was independent prognostic factor for relapse-free survival (P=0.042) and overall survival (P=0.001).
Colorectal cancer (CRC) is the third most common cancer worldwide with over 1.8 million new cases in 2020 [1]. Per the latest trends, the populations are getting older in the developed countries, therefore the numbers of older patients with CRC undergoing surgery are increasing. In CRC, surgery remains the most useful curative treatment, although tumor recurrence occurs at a constant rate after the curative resection [2]. However, predicting the outcomes of patients with CRC undergoing curative surgery remains a major challenge. Furthermore, identification of the predictors of recurrence and poor prognosis may lead to better management and treatment, and could improve the outcomes of such patients.
There is a large body of evidence that suggests chronic inflammation plays an important role in carcinogenesis, malignant progression of tumors, and recurrence of cancer. Systemic inflammatory scoring systems, such as the modified Glasgow Prognostic Score (mGPS), neutrophil to lymphocyte ratio, platelet to lymphocyte ratio, and lymphocyte to monocyte ratio have been reported as useful predictors of survival in patients with various solid tumors [3–6]. Recently, the C-reactive protein (CRP) to albumin ratio (CAR) has demonstrated prognostic utility in patients with several types of cancer, including CRC [7]. The CAR is a simple scoring system that is based on serum CRP and albumin levels. CRP is an acute-phase protein synthesized in the liver on activation of tumor necrosis factor α (TNF-α) and interleukin 6 (IL-6) , and several studies have shown the association of elevated serum CRP levels with poor prognosis in various cancers, including CRC [8, 9]. However, whether CAR is associated with outcomes in older patients CRC has not yet been elucidated. The aim of this study was, therefore, to examine the predictive and prognostic value of the preoperative CAR in older patients with CRC undergoing curative resection.
This study was approved by the Institutional Review Boards of Hiratsuka Kyosai Hospital (No. 2-18) and Yokohama Minami Kyosai Hospital (No. 2-23). Written informed consent was obtained from all patients before surgery. The study protocol conformed to the ethical guidelines of the 2013 Declaration of Helsinki, according to the Institutions’ human research committees [10].
A total of 244 older patients (75 years and over, 119 men and 125 women) who underwent curative resection at Hiratsuka Kyosai Hospital and Yokohama Minami Kyosai Hospital in Japan between January 2008 and December 2016 were included in this retrospective study. The inclusion criteria were as follows: (1) 75 years or older; (2) pathological stage (pStage) II or III CRC; (3) underwent R0 resection for CRC as primary treatment; and (4) biochemical profiles, including the serum albumin, and CRP levels were measured within 1 month before the surgery. The pStage I CRC has a low recurrence rate and was considered to be of little importance in the study; thus, patients with stage I CRC were excluded from this study. The exclusion criteria were as follows: (1) emergency operation; (2) synchronous cancer; (3) existence of penetration or perforation; (4) severe liver cirrhosis; and (5) nephrotic syndrome. The CAR was calculated as the ratio of the serum CRP (mg/dL) to the serum albumin (g/dL). Tumor staging was conducted according to the Japanese Classification of Colorectal Carcinoma (9th edition, 2019). The World Health Organization (WHO) defines people aged 65 to 74 years as early-stage older people and those aged 75 years or older as late-stage older people. In recent years, there have been other reports that consider people aged 75 years or over as older people [11]. Therefore, in the present study, patients aged 75 years or over were defined as older individuals.
For patients with pStage III CRC or high-risk pStage II CRC, adjuvant chemotherapy is recommended. The criteria for high-risk pathological stage II were pT4, poorly differentiated histology, presence of lymphovascular invasion, presence of perineural invasion, bowel obstruction, less than 12 lymph nodes evaluated in the pathology report, or close or indeterminate margins, according to the NCCN guidelines [12]. The following 6 regimens were used as postoperative adjuvant chemotherapy: fluorouracil plus leucovorin (5-FU/LV); capecitabine; uracil-tegafur plus leucovorin (UFT/LV); tegafur/gimeracil/oteracil/potassium (S-1); 5-FU/LV plus oxaliplatin (FOLFOX); and capecitabine plus oxaliplatin (CAPOX).
Patients who underwent surgery had follow-up visits every 3 months during the first 3 years, and every 6 months over the next 2 years. A physical examination and serum carcinoembryonic antigen (CEA) measurements were performed at each visit. The chest and abdominopelvic computed tomography scans were obtained every 6 months. All patients were regularly followed up with colonoscopy every 1 to 2 years.
The optimal cutoff value of the CAR was identified via the receiver operating characteristics (ROC) curve. The significance of association between the CAR and the clinicopathological characteristics were assessed using the Fisher exact test. The cumulative relapse-free survival (RFS) and overall survival (OS) rates were estimated according to the Kaplan-Meier method and compared using the log-rank test. The predictors of outcomes were assessed using univariate and multivariate analyses via Cox proportional hazard models. The significant prognostic factors identified in univariate analysis (P-values of <0.10) were selected for multivariate analysis. P-values were derived from 2-tailed tests. For all statistical tests, the level of significance was set at 0.05 and all statistical analyses were performed using the EZR software program (Saitama Medical Center, Jichi Medical University), a graphical user interface for R ver. 2.13.0 (R Foundation for Statistical Computing) or, more precisely, a modified version of R commander ver. 1.8-4 designed to add statistical functions frequently used in biostatistics [13].
The baseline clinical characteristics of the patients are shown in Table 1. The median follow-up period was 50.8 months (range, 1.1–137.0 months). Of the 244 patients, 104 (42.6%) had pII-stage disease, and 140 (57.4%) had pIII-stage disease. A total of 57 of the 244 patients (23.4%) displayed tumor recurrence after surgery.
The median preoperative CAR was 0.068, with a range of 0.0003 to 3.91. To investigate the cutoff value for the preoperative CAR, we used ROC curve analysis (Fig. 1), and we found the appropriate cutoff value of 0.085 (sensitivity of 65.7%, specificity of 60.3%), based on which the patients were divided into high-CAR group (CAR ≥0.085) and low-CAR group (CAR <0.085).
The associations between CAR and clinicopathological characteristics were assessed and are presented in Table 2. The CAR ranged from 0.0003 to 3.91 (median, 0.068). The present study revealed that high CAR was significantly associated with high CEA levels (P=0.001), a larger tumor size (P<0.001), and advanced pT factor (P=0.001).
Patients with high CAR had significantly shorter RFS and OS values than did the patients with low CAR (P=0.015 and P<0.001, respectively, according to the log-rank test) (Fig. 2). Univariate Cox proportional analysis showed CEA level of ≥5.0 ng/mL (P=0.016), high CAR (P=0.002), pT4 (P<0.001), lymph node metastasis (P=0.008), and lymphatic invasion (P=0.001) to be significant factors predicting poor RFS. The multivariate analysis of these variables indicated that high CAR (P=0.042), pT4 (P=0.017), and lymphatic invasion (P=0.020) were independent predictors of poor RFS (Table 3). While analyzing OS, the univariate analysis indicated that CEA level of ≥5.0 ng/mL (P=0.042), high CAR (P<0.001), pT4 (P=0.017), and lymphatic invasion (P=0.005) were significantly correlated with poor OS. The multivariate analysis indicated that high CAR (P=0.001) was the independent predictor of poor OS (Table 4).
The present study on older patients with pStage II or III CRC who underwent curative surgery revealed that elevated CAR was related to the factors related to tumor progression such as CEA, tumor size, and pT factor. These results are in accordance with the result of a meta-analysis in CRC [7] that demonstrated elevated CAR to be related to high CEA, and larger tumor size. We also revealed that elevated CAR was significantly associated with shorter RFS and OS, which is consistent with the results of recent studies that showed the prognostic and/or predictive value of the CAR in various types of cancer [14–16]. Additionally, these results are also consistent with studies reporting that elevated CAR was significantly associated with a poor prognosis among CRC patients with inoperable disease and/or those undergoing surgery [7, 17, 18].
In addition, tumor progression causes cachexia and activates cytokines, such as IL-1β, IL-6, and TNF-α that suppress the gene expression of albumin [19]. This results in hypoalbuminemia, and low albumin levels have been associated with poor prognosis in various cancer [20, 21]. Therefore, the CAR can be considered to be a good indicator for assessing the status of both inflammation and nutrition.
Similar to CAR, the mGPS is also based on CRP and albumin, and has been reported to be a useful prognostic marker in various malignant tumors [22–24]. The disadvantage of utilizing an mGPS is that it is considered to be a discontinuous variable; thus, it is not possible to evaluate small differences. Therefore, mGPS may overestimate or underestimate the level of inflammation.
Moreover, since the majority of the patients are classified into mGPS 0 or 1, mGPS could not effectively distinguish the survival differences of most of the patients [25, 26]. Similarly, in this study, approximately 85% of patients were classified with a 0 or 1 score. Hence, we chose CAR rather than mGPS as a prognostic factor in this study.
While the number of articles about CAR has increased recently, there were few studies that investigated the utility of CAR in older patients with malignant tumors. Considering the aging of population in the recent years, it is important to evaluate the impact of inflammation-based prognostic scores in older patients with CRC. In this study, the median CAR level was higher in the older group (Table 1). It has been reported that the levels of inflammatory markers increase with increasing age [27]; therefore, it may be preferable to establish an evaluation method considering adjustment according to age in the future.
What should be done for cases with elevated CAR levels? In these cases, it may be better to perform interventions during the perioperative period to improve prognosis. Our results showed that elevated CAR level was associated with CEA level (≥5 ng/mL), tumor size (≥50 mm), and pT factor (pT4). In these cases, preoperative treatment (chemotherapy and/or radiotherapy) may be useful for lowering tumor marker levels and shrinking tumors. In addition, studies suggested the use of exercise therapy as anti-inflammatory therapy [28, 29]. Additionally, randomized controlled trial [30] and systematic review [31] have suggested that perioperative nutrition therapy, synbiotic treatment, and preoperative immune modulator nutrition reduce postoperative infectious complications. There have been multiple reports that postoperative inflammatory complications worsen prognosis; hence, there is a possibility that improvement in prognosis can be expected by reducing the incidence of postoperative inflammatory complications. In the future, it is desirable to conduct randomized controlled trials in which these nutritional or exercise therapies are administered to patients with a poor preoperative inflammatory status.
There were certain limitations and problems in the current study. First, this was a retrospective study with relatively small sample size. Second, the cutoff point for CAR might be variable based on the sample size, and our cutoff value for CAR was biased because of being selected via ROC curve. Third, potential introducing bias should also be considered because, in some cases, the introduction of adjuvant chemotherapy was not performed because the attending physician did not recommend it. Finally, it is possible that the results may have been different by adding early-stage I cases. Therefore, further large-scale prospective cohorts are warranted and it is important to determine an appropriate cutoff point.
In conclusion, an elevated preoperative CAR appears to be a useful and promising predictor of poor outcomes in older patients with CRC undergoing potentially curative surgery.
Fig. 1.
Receiver operating characteristic analysis of the C-reactive protein to albumin ratio (CAR) for survival status. Area under the curve of the CAR is 0.65.
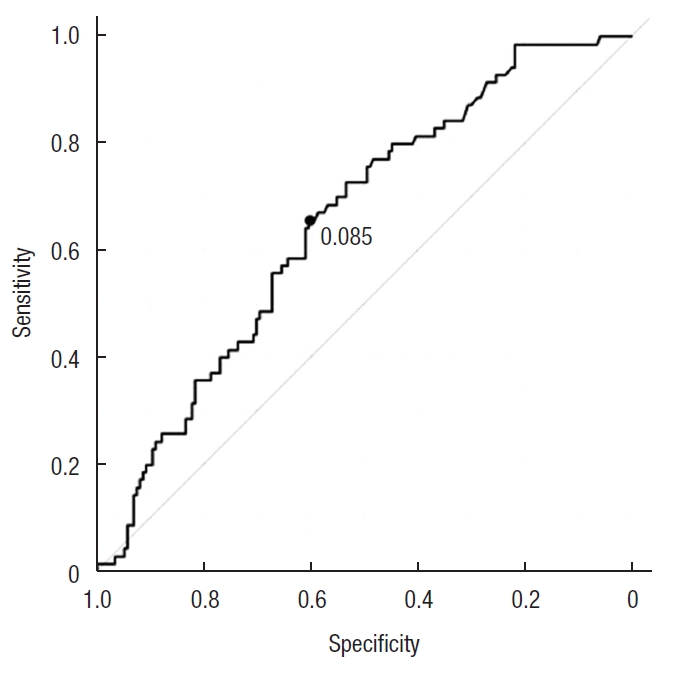
Fig. 2.
Kaplan-Meier survival plots compared by the log-rank test. (A) Relapse-free survival (RFS) curves based on the C-reactive protein to albumin ratio (CAR). The 3-year RFS rates of the patients with low CAR (solid line) and high CAR (dotted line) were 85.8% and 66.4%, respectively. (B) Overall survival (OS) curves based on the CAR. The 3-year OS rates of the patients with low CAR (solid line) and high CAR (dotted line) were 87.4% and 71.0%, respectively.
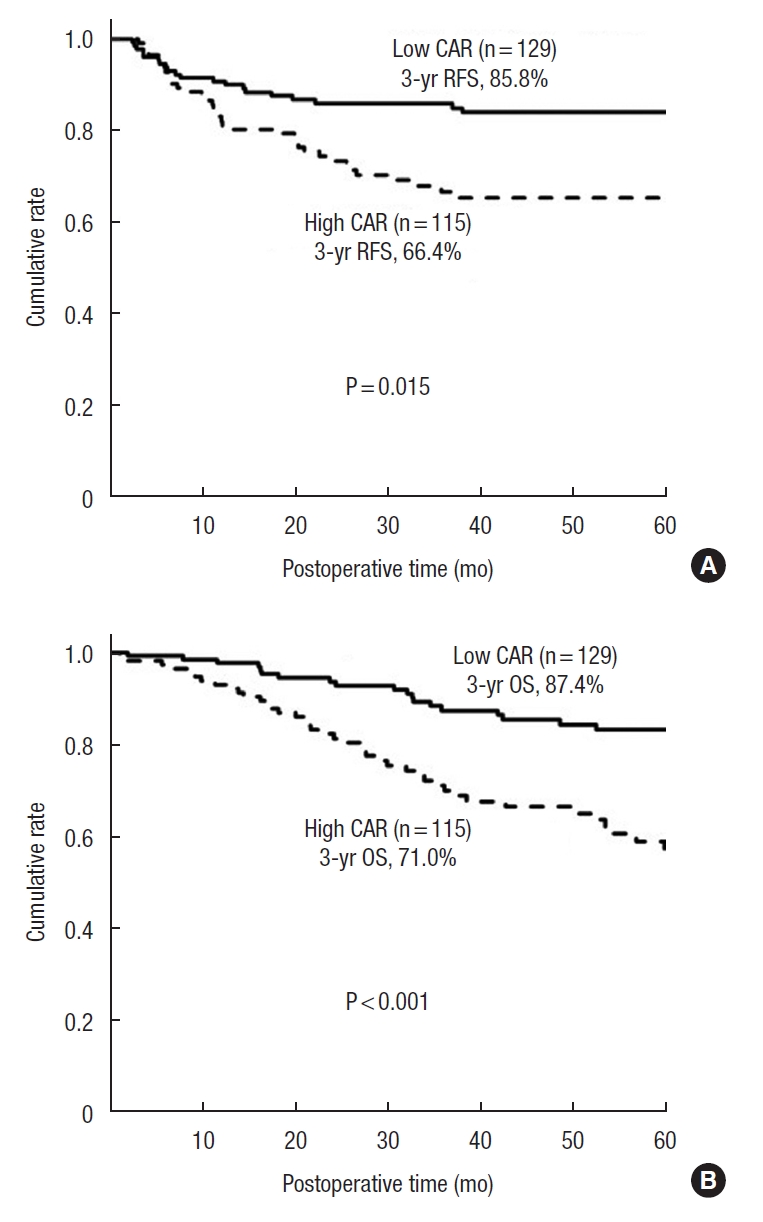
Table 1.
Patients’ characteristics (n=244)
| Characteristic | Value |
|---|---|
| Age (yr) | 81 (75–99) |
| Sex | |
| Male | 119 (48.8) |
| Female | 125 (51.2) |
| Tumor location | |
| Colon | 192 (78.7) |
| Rectum | 52 (21.3) |
| CAR | 0.068 (0.0003–3.91) |
| Median of CAR by age (yr) | |
| 75–81 | 0.055 (0.0003–3.82) |
| ≥82 | 0.088 (0.002–3.91) |
| Type of surgery | |
| Partial colectomy | 118 (48.4) |
| Hemicolectomy | 62 (25.4) |
| (Rectum) anterior resection | 48 (19.7) |
| Hartmann | 10 (4.1) |
| Abdominoperineal resection | 6 (2.4) |
| Pathological stagea) | |
| II | 104 (42.6) |
| III | 140 (57.4) |
| Follow-up (mo) | 50.8 (1.1–137.0) |
| Recurrence | |
| No | 187 (76.6) |
| Yes | 57 (23.4) |
Table 2.
Relationship between CAR and clinicopathological variables
Table 3.
Univariate and multivariate analysis for predictors of relapse-free survival (n=244)
Table 4.
Univariate and multivariate analysis for predictors of overall survival (n=244)
REFERENCES
1. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2021;71:209–49.



2. Van Cutsem E, Nordlinger B, Adam R, Köhne CH, Pozzo C, Poston G, et al. Towards a pan-European consensus on the treatment of patients with colorectal liver metastases. Eur J Cancer 2006;42:2212–21.


3. Bowen RC, Little NA, Harmer JR, Ma J, Mirabelli LG, Roller KD, et al. Neutrophil-to-lymphocyte ratio as prognostic indicator in gastrointestinal cancers: a systematic review and meta-analysis. Oncotarget 2017;8:32171–89.



4. Jin J, Hu K, Zhou Y, Li W. Clinical utility of the modified Glasgow prognostic score in lung cancer: a meta-analysis. PLoS One 2017;12:e0184412.



5. Wang X, Ni X, Tang G. Prognostic role of platelet-to-lymphocyte ratio in patients with bladder cancer: a meta-analysis. Front Oncol 2019;9:757.



6. Gu L, Li H, Chen L, Ma X, Li X, Gao Y, et al. Prognostic role of lymphocyte to monocyte ratio for patients with cancer: evidence from a systematic review and meta-analysis. Oncotarget 2016;7:31926–42.



7. Zhou QP, Li XJ. C-reactive protein to albumin ratio in colorectal cancer: a meta-analysis of prognostic value. Dose Response 2019;17:1559325819889814.




8. Kobayashi T, Teruya M, Kishiki T, Endo D, Takenaka Y, Tanaka H, et al. Inflammation-based prognostic score, prior to neoadjuvant chemoradiotherapy, predicts postoperative outcome in patients with esophageal squamous cell carcinoma. Surgery 2008;144:729–35.


9. Kim WR, Han YD, Min BS. C-reactive protein level predicts survival outcomes in rectal cancer patients undergoing total mesorectal excision after preoperative chemoradiation therapy. Ann Surg Oncol 2018;25:3898–905.



10. World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA 2013;310:2191–4.


11. Hirashima K, Watanabe M, Shigaki H, Imamura Y, Ida S, Iwatsuki M, et al. Prognostic significance of the modified Glasgow prognostic score in elderly patients with gastric cancer. J Gastroenterol 2014;49:1040–6.



12. National Comprehensive Cancer Network (NCCN). NCCN clinical practice guidelines in oncology: rectal cancer. Version 1. NCCN Foundation; 2024.

13. Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant 2013;48:452–8.




14. Yang X, Liu H, He M, Liu M, Zhou G, Gong P, et al. Prognostic value of pretreatment C-reactive protein/albumin ratio in nasopharyngeal carcinoma: a meta-analysis of published literature. Medicine (Baltimore) 2018;97:e11574.



15. Kunizaki M, Tominaga T, Wakata K, Miyazaki T, Matsumoto K, Sumida Y, et al. Clinical significance of the C-reactive protein-to-albumin ratio for the prognosis of patients with esophageal squamous cell carcinoma. Mol Clin Oncol 2018;8:370–4.



16. Di QS, Xu T, Song Y, Zuo ZG, Cao FJ, Yu XJ, et al. High C-reactive protein to albumin ratio predicts inferior clinical outcomes in extranodal natural killer T-cell lymphoma. Dose Response 2020;18:1559325820917824.




17. Ishizuka M, Nagata H, Takagi K, Iwasaki Y, Shibuya N, Kubota K. Clinical significance of the C-reactive protein to albumin ratio for survival after surgery for colorectal cancer. Ann Surg Oncol 2016;23:900–7.



18. Shibutani M, Maeda K, Nagahara H, Iseki Y, Hirakawa K, Ohira M. The significance of the C-reactive protein to albumin ratio as a marker for predicting survival and monitoring chemotherapeutic effectiveness in patients with unresectable metastatic colorectal cancer. Springerplus 2016;5:1798.




19. Chojkier M. Inhibition of albumin synthesis in chronic diseases: molecular mechanisms. J Clin Gastroenterol 2005;39(4 Suppl 2):S143–6.


20. Borda F, Borda A, Jiménez J, Zozaya JM, Prieto C, Gómez M, et al. Predictive value of pre-treatment hypoalbuminemia in prognosis of resected colorectal cancer. Gastroenterol Hepatol 2014;37:289–95.


21. Crumley AB, Stuart RC, McKernan M, McMillan DC. Is hypoalbuminemia an independent prognostic factor in patients with gastric cancer? World J Surg 2010;34:2393–8.



22. Wang F, He W, Jiang C, Guo G, Ke B, Dai Q, et al. Prognostic value of inflammation-based scores in patients receiving radical resection for colorectal cancer. BMC Cancer 2018;18:1102.




23. Tian R, Zhang F, Sun P, Wu J, Yan H, Wu AR, et al. The preoperative sensitive-modified Glasgow prognostic score is superior to the modified Glasgow prognostic score in predicting long-term survival for esophageal squamous cell carcinoma. Oncotarget 2016;7:67485–94.



24. Jamieson NB, Denley SM, Logue J, MacKenzie DJ, Foulis AK, Dickson EJ, et al. A prospective comparison of the prognostic value of tumor- and patient-related factors in patients undergoing potentially curative surgery for pancreatic ductal adenocarcinoma. Ann Surg Oncol 2011;18:2318–28.



25. Shibutani M, Maeda K, Nagahara H, Iseki Y, Ikeya T, Hirakawa K. Prognostic significance of the preoperative ratio of C-reactive protein to albumin in patients with colorectal cancer. Anticancer Res 2016;36:995–1001.


26. He X, Li JP, Liu XH, Zhang JP, Zeng QY, Chen H, et al. Prognostic value of C-reactive protein/albumin ratio in predicting overall survival of Chinese cervical cancer patients overall survival: comparison among various inflammation based factors. J Cancer 2018;9:1877–84.



27. Wyczalkowska-Tomasik A, Czarkowska-Paczek B, Zielenkiewicz M, Paczek L. Inflammatory markers change with age, but do not fall beyond reported normal ranges. Arch Immunol Ther Exp (Warsz) 2016;64:249–54.




28. Gleeson M, Bishop NC, Stensel DJ, Lindley MR, Mastana SS, Nimmo MA. The anti-inflammatory effects of exercise: mechanisms and implications for the prevention and treatment of disease. Nat Rev Immunol 2011;11:607–15.



29. Oubaya N, Soubeyran P, Reinald N, Fonck M, Allain M, Zebachi S, et al. Prognostic value of routinely measured inflammatory biomarkers in older cancer patients: pooled analysis of three cohorts. Cancers (Basel) 2021;13:6154.



- TOOLS
-
METRICS

-
- 4 Crossref
- Scopus
- 1,859 View
- 45 Download
- Related articles in ACP
-
Prognostic Significance of Lymph Node Ratio in Stage III Rectal Cancer2011 October;27(5)