INTRODUCTION
Obstetric perineal laceration with ano-rectal sphincter (ARS) disruption remains the most common cause of fecal incontinence (FI) among women worldwide. Management of complex perineal trauma has been a subject of extensive research since no current treatment options have provided effective long-term results [1]. The overlapping sphincteroplasty, which is considered the standard surgical procedure for Obstetric Anal Sphincter Injuries (OASIS), has disappointing results in the long-term [1, 2]. Recently, a perineal transposed antropyloric valve (APV) for total anorectal reconstruction has been described for excised or severely damaged ARS as an alternative to permanent colostomy [3]. To our knowledge, the present report is the first to describe the use of transposed APV for perineal reconstruction in a case of complex OASIS.
CASE REPORT
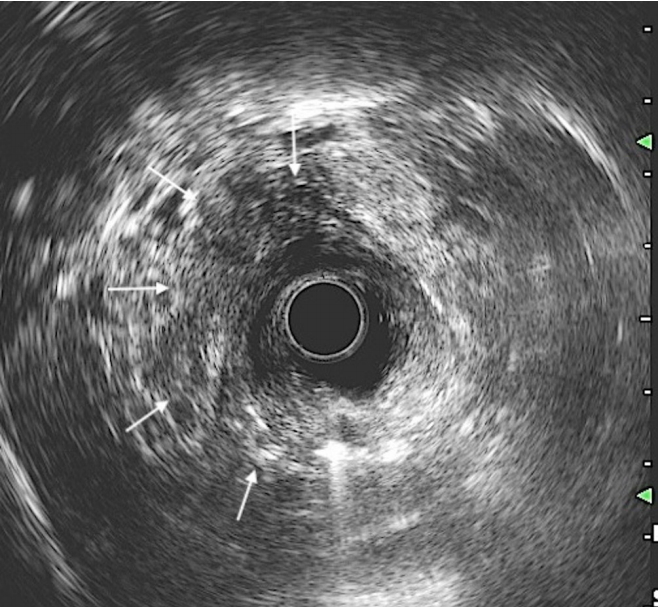
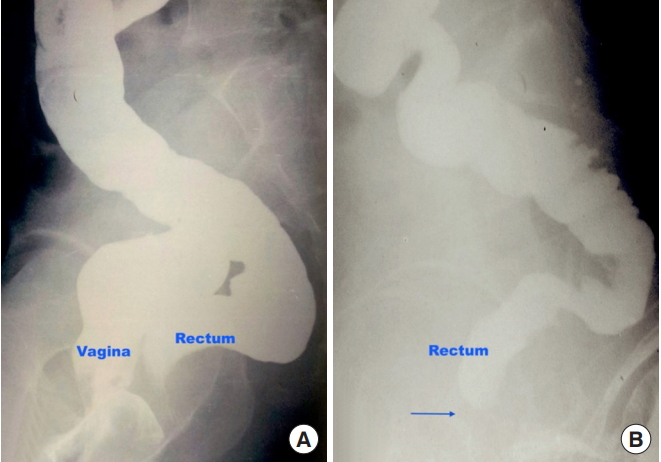
A 24-year-old primipara presented to us with a 3-week-old third-degree perineal tear and OASIS. The delivery was conducted at a remote primary health care center; an episiotomy was not performed. The patient had developed complete FI following injury. Because of the injury severity, a primary repair of the perineal laceration was not attempted. A diverting loop colostomy was created one week after delivery, and the patient was referred to us for definitive management. The patient was otherwise healthy and had no comorbidities or any significant past medical or surgical history. The patient was psychologically distressed by the loss of her child and because of the newly created abdominal stoma. General and systemic examinations were unremarkable. She weighed approximately 60 kg and had a body mass index of 24 kg/m2. On perineal examination, anal tone was diminished and a large communication between the rectum and vagina could be visualized 2 cm above the anal verge. A per-vaginal speculum examination revealed a fistulous opening on the posterior wall with surrounding mucosal erythema. Communication could be easily demonstrated by a per-rectal examination as well (Fig. 1). Three-dimensional endoanal ultrasound was conducted, which showed severely damaged ARS (both internal and external sphincters, > 180°) in the anterolateral position (Fig. 2).
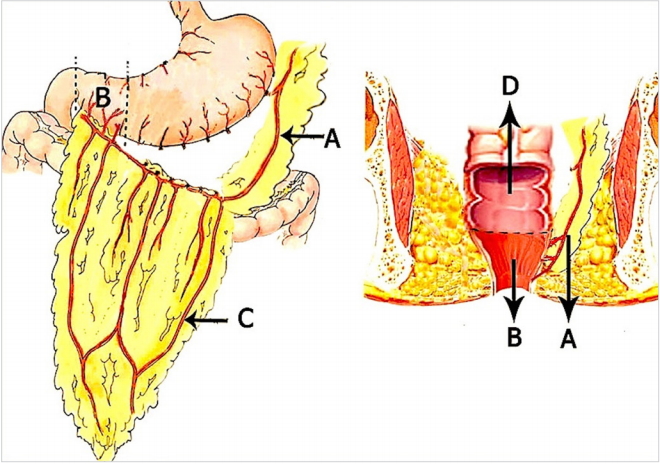
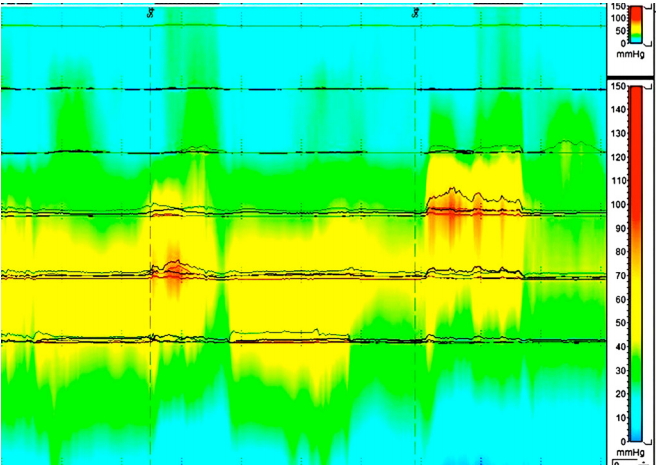
Because of the irreparably damaged ARS, the patient was offered APV transposition for anal reconstruction. We conducted this procedure in compliance with the principles of the Declaration of Helsinki. The operative protocol was reviewed and approved by the Institutional Review Board (IRB) of the King George’s Medical University, Lucknow, Uttar Pradesh, India (IRB No. 1206/Rcell-10 dated 18-08-2010). Written informed consent was obtained from the patient. The surgery was performed under spinal anaesthesia in the lithotomy position. A midline laparotomy incision was created. Gastrocolic omentum was mobilised close to the transverse colon. Hepatic flexure of the colon was mobilized and the duodenum was kocherized. Branches of the gastroepiploic arcade to the greater curvature of the stomach were serially ligated and divided, which safeguarded the terminal branches to the antropyloric region. The right gastroepiploic artery was divided, which preserved the infrapyloric branches. The APV was then mobilized based on the left gastroepiploic pedicle after dividing its antral and duodenal ends. Pelvic dissection was initiated by removing the intrapelvic adhesions, and the rectum was mobilized to the pelvic floor. The fistulous communication between the rectum and vagina was identified and deconstructed. The defect on the vaginal side was closed with polyglactin 2-0 sutures in a single continuous layer. The rectum was divided at the fistula level, and the edges were debrided. The antral end of the mobilized APV segment was then sutured to the proximal rectal end with interrupted silk 2-0 sutures (Fig. 3). The graft was invaginated through the distal rectal cuff, and the duodenal end was sutured to the freshened perianal skin. A movie file has been provided to illustrate the steps of the procedure. The proximal colostomy was retained. Bowel continuity was maintained with retrocolic posterior gastrojejunostomy. Postoperative recovery was fairly unremarkable, and the patient had clinically good neoanal sphincter tone. The patient had mild surgical wound infection, which was managed conservatively. Oral feeding was initiated gradually, and the patient was discharged 9 days after surgery. A clinical and neoanal manometric examination performed at the 1-month follow-up displayed good sphincter pressures with a resting pressure of 58 mmHg and maximum squeeze pressure of 74 mmHg (Fig. 4). A distal colonic loop barium retention study was performed through the colostomy that showed a smooth beak impression of the APV graft with holding of barium proximal to it on late films (Fig. 5). The diverting colostomy was closed 3 months after surgery. One month after colostomy closure, the patient’s St. Mark’s incontinence score was seven, which indicates good sphincter control. The patient was followed-up for 36 months during which the patient remained satisfied with the surgery outcome and maintained a fairly good continence status. The patient developed no long-term complications related to gastrectomy. Persistent mucous discharge from the duodenal end of the graft was initially a problem but gradually subsided over time.
DISCUSSION
Globally, OASIS is the leading cause of FI among young women. It has been estimated that between 4% and 6% of women having a vaginal delivery suffer from FI [4]. Commonly, these injuries occur due to a prolonged second stage of labor, which results in pressure necrosis of the rectovaginal septum. The patient in this study had obstructed labor that resulted in severe perineal laceration with a rectovaginal fistula and resulted in the death of the patient’s baby.
The incidence of underlying ARS injury in patients with obstetric perineal trauma and rectovaginal fistula is estimated to be very high [2]. Therefore, meticulous sphincter evaluation in these patients using endo-rectal ultrasound and/or manometric study is justified [5]. The patients clinically present with fecal, gaseous, or mucus discharge through the vagina along with symptoms of FI.
Management of complex obstetric perineal injury still remains a challenge and often requires specialized and multidisciplinary care. Currently, surgical treatment with overlapping sphincteroplasty is considered the standard of care. Though the reported short-term results of this procedure are good (74% of improved continence at three months), the long-term outcome is suboptimal. Larger studies with follow-ups of more than 5 years have consistently shown that only half of the patients undergoing sphincteroplasty remained continent in the long-term [6, 7]. Furthermore, in our patient sphincteroplasty was not suitable as the sphincter was irreparably damaged and only native sphincter tissue fibrosis was present. In similar situations when the anal sphincter is severely damaged, skeletal muscles (gracilis, gluteus maximus) have also been used as wraps around the anus to augment ARS function, but with less satisfactory outcomes [8, 9]. Dynamic graciloplasty (converting type II to type I fibers) and artificial bowel sphincter implantation have also been attempted, but with limited success and significant associated morbidity [9, 10]. The role of sacral nerve stimulation in the management of traumatic FI is being explored and has been found to be effective in patients with partial ARS tears [11]. Still today, there are no satisfactory options for anal reconstruction that are an alternative to a permanent colostomy in patients with severely damaged ARS.
Permanent colostomy may offer good long-term quality of life (QoL) for patients with end-stage FI, although data are lacking from the developing world. Living with a permanent colostomy is an undesired outcome due to the social stigma in Asia. Moreover, the inability to receive proper stoma care along with the life-long need to purchase stoma appliances are issues that make colostomy unfavorable [12]. In the present case, when the patient was given a choice, she readily opted for perineal reconstruction with APV transposition.
Perineal transposition of APV is a novel technique for total anorectal reconstruction in patients with severely damaged/excised ARS complex. It is hypothesized that this fatigue resilient smooth muscle segment may provide an appropriate substitute for native ARS because prolonged tonic contraction is provided [13]. In a recently published study on initial outcomes of APV transposition in patients with severe FI, most of the patients showed an increase in anal manometric pressures with improvements in their postoperative incontinence and QoL scores [3]. The transposed antropylorus behaves like an obstructive ring at the perineal outlet but lacks voluntary control. In our previous study, the postoperative functional result and QoL were better in patients with an intact rectum and sensate anal canal compared to the excision group [3]. Moreover, the gluteus maximus is a strong and bulky muscle that acts as a natural accessory anal contractor. Many patients gradually learn to use their gluteus muscle as an accessory mechanism for voluntary fecal control.
The potential long-term complications of gastrojejunostomy (dumping syndrome, downstream acid injury, and alkaline reflux syndrome) remain a valid concern, though the actual incidence has been reported as low [3, 14]. Our patient did not have any of these complications in the postoperative follow-up. Initially the patient had to apply perineal pads due to persistent mucus discharge from the duodenal end of the graft, which gradually decreased over time. At the 3-year follow-up, the patient had fairly good continence status (St. Mark’s incontinence score of 7) and overall procedure-related satisfaction.
Perineal APV transposition can be an effective alternative to a permanent colostomy in patients with complex obstetric perineal injury and associated ARS damage. This technique, though feasible and effective in the preliminary evaluation, is technically demanding and needs to be performed in a surveillance setting. Lack of long-term results and the complex nature of surgery may preclude routine use of this procedure at present, although it is a promising technique that opens a new dimension in the management of intractable FI.