- Search
| Ann Coloproctol > Volume 34(6); 2018 > Article |
|
Abstract
Purpose
Hartmann operation is widely recognized as a useful procedure, especially in emergencies involving the rectosigmoid colon. One of the surgeonŌĆÖs foremost concerns after Hartmann operation is future colostomy reversal, as colostomy reversal after a Hartmann procedure is associated with relatively high morbidity and mortality. Laparoscopic surgical techniques continue to prove useful for an ever-increasing variety of indications. We analyzed the outcomes of laparoscopic Hartmann colostomy reversals at our center.
Methods
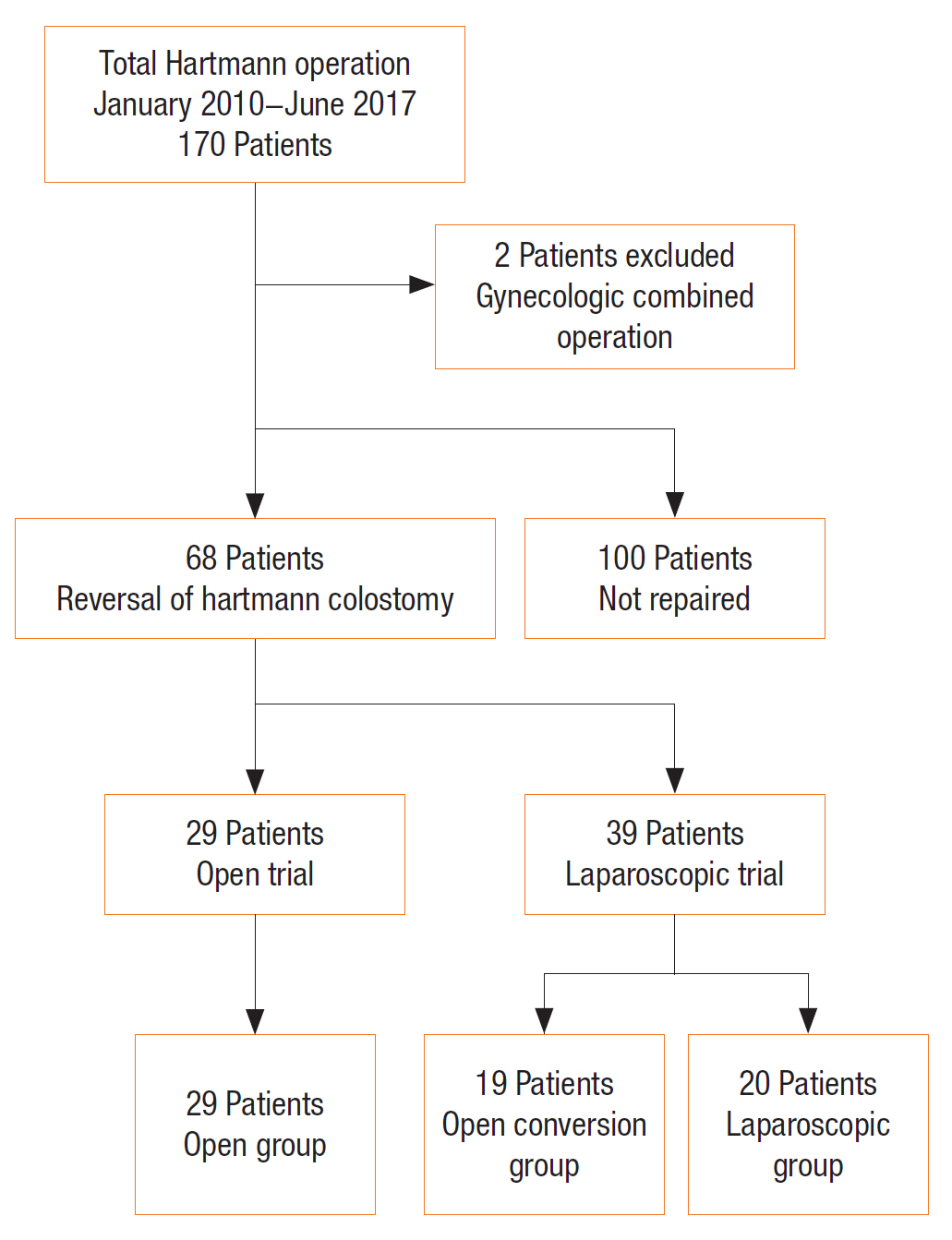
We retrospectively analyzed the hospital records of 170 patients who had undergone Hartmann operation between January 2010 and June 2017 at Wonkwang University Hospital. Among 68 Hartmann colostomy reversals, we evaluated and compared the outcomes of 3 groups of patients: 29 patients in the open colostomy reversal group (OG) who had undergone laparotomies for Hartmann reversals, 19 patients in the conversion group (CG) whose laparoscopic procedures had required conversion to a laparotomy, and 20 patients in the laparoscopy group (LG).
Results
The overall reversal rate for Hartmann colostomies was 40.5% during this time period. The duration of hospital stay was significantly shorter among LG patients (10.15 ┬▒ 2.94 days) than among OG patients (16 ┬▒ 9.5 days). The overall complication rate among OG patients was higher than that among LG patients (adjusted odds ratio, 8.78; P = 0.01). The most common complication was postoperative ileus (19.1%).
The French surgeon Henri Albert Hartmann first described his eponymous operation in 1921. Since then, Hartmann operation has been widely used to treat or palliate patients with rectosigmoid pathologies. More recently, however, the procedure has generally been reserved for emergencies when primary anastomosis is not possible [1] and is usually performed on unprepared bowel segments and on patients who have sepsis or multiorgan dysfunction. For most patients, a colostomy reversal operation is required to address stoma-related quality-of-life impairment. After recovery from the initial surgery, colostomy reversal and restoration of bowel continuity are indicated in selected patients (those who are not at risk of severe adhesions or other complications). Hartmann colostomy reversal is a major surgical procedure associated with significant morbidity and mortality from complications such as anastomotic leakage and surgical wound infection [2-4].
Recently, laparoscopic colon surgery, including laparoscopic Hartmann colostomy reversal, has become more common. However, restoration of bowel continuity after a Hartmann operation carries a risk of significant morbidity, with reported anastomotic leak rates of 4% to 16% and mortality rates of up to 10% [4]. Therefore, laparoscopic techniques have been applied to colostomy reversal to reduce morbidity and mortality. Initial small laparoscopic series have reported zero deaths, as well as shorter lengths of hospitalization and lower morbidity than open colostomy reversal series [4, 5]. Herein, we report our up-to-date experience with laparoscopic reversal of HartmannŌĆÖs operation to assess its efficacy and safety compared to open reversal.
We retrospectively collected data from the medical records of patients who had undergone Hartmann operation between 2010 and June 2017 at Wonkwang University Hospital. Over these 7.5 years, 170 patients underwent Hartmann operation. We excluded 2 trauma patients who had experienced multiple organ injuries requiring multiple corrective procedures. Among the 168 records included in the analysis, 68 patients (40.5%) had undergone reversal of Hartmann operation (Fig. 1). We categorized the 29 patients who had undergone laparotomies for Hartmann reversal into the open reversal group (OG). Twenty patients (the laparoscopy group [LG]; single port for 9 patients and a conventional procedure for 11 patients) had undergone laparoscopic colostomy reversal. Nineteen patients (the conversion group [CG]) had experienced intraoperative conversion of their colostomy reversal procedures from laparoscopy to laparotomy. This study was approved by the Institutional Review Board of Wonkwang University Hospital (approval number: 2017-05-023), which waived the requirement for informed consent in this retrospective study.
For comparison among the patient groups, outcome variables were the number of patients, patientŌĆÖs age, sex, and body mass index (BMI), comorbidities (diabetes mellitus or hypertension), American Society of Anesthesiologists (ASA) physical status classification, indication for previous Hartmann operation, previous operation type (open vs. laparoscopy), mean operation time, conversion to open surgery, length of hospital stay, mortality, and complications. The results were analyzed using the 1-way analysis of variance, the chi-square test, Scheffe multiple comparison test, and Fisher exact test in IBM SPSS ver. 18.0 (IBM Co., Armonk, NY, USA). Any differences among the three groups were considered statistically significant if the P-value was <0.05.
Laparoscopy was performed with the patient in a modified lithotomy position. The first step was takedown of the colostomy. Peristomal adhesiolysis was done through the previous colostomy site. After colostomy takedown, the head of a circular stapler was installed at the opening of the proximal colon. Then, a single laparoscopic port was inserted into the colostomy site and used to create a pneumoperitoneum. Then, the laparoscope was used to observe the intra-abdominal condition, particularly the location and density of adhesions near the distal colonic (or rectal) stump. For patients in whom single-port laparoscopy was difficultŌĆöowing to severe intra-abdominal adhesionsŌĆöan additional one to three trocars were inserted, as needed. A circular stapler was then introduced transanally, and colorectal intracorporeal anastomosis was performed under laparoscopic guidance. If necessary, a rectal tube was inserted through the anus for decompression. Reinforcement sutures were applied in most patients. The trocar insertion sites were sutured with 3/0 Vicryl. Finally, the colostomy opening in the abdominal wall was closed.
The indications for Hartmann operation among patients in the three groups were colon cancer, diverticular perforation, stercoral perforation, traumatic colon injury, ischemic colitis, postoperative adhesions, and sigmoid volvulus. Irrespective of operative method, the most common indications for Hartmann operation was colon cancer (57.3%). The second most common indication was diverticular disease (16.1%). No statistically significant preponderance of one indication or another was identified among the 3 groups (Table 1).
No statistically significant differences in age, sex, BMI, and comorbid diseases (diabetes mellitus, hypertension) were found among the 3 groups. In addition, the mean ASA physical status was not significantly different among the 3 groups (P = 0.58). The operation time was defined as the time interval between the start of general anesthesia and the patientŌĆÖs arrival in the recovery room postoperatively. The mean operation times for OG, CG, and LG patients were, respectively, 222.5 ┬▒ 95.5, 234.6 ┬▒ 74.7, and 224.3 ┬▒ 83.5 minutes (P = 0.88) (Table 2). The mean duration of admission among LG patients was 5.8 days shorter than that among OG patients. CG patients were hospitalized for longer than LG patients, but this difference was not statistically significant based on Scheffe multiple comparision test (Table 3). To understand the effect of laparoscopic attempts on outcome, we compared a laparoscopic trial group to the open group; we found no significant differences in any of the variables between the 2 groups. Nevertheless, the hospital stay of the laparoscopic trial group was 4.2 days shorter than that of the open group (Table 4).
Overall, the postoperative complication rate among patients who underwent reversal of Hartmann operation was 35.3%. The most common complication was postoperative ileus (13 patients, 19.1%), the detection of which was supported by assessing abdominal X-rays. Postoperative ileus was reported for 8 OG patients and 1 LG patient. All patients with postoperative ileus improved with conservative management. Wound-related complications also affected 8 OG patients and 1 LG patient. Fourteen OG patients, 12 CG patients, and 18 LG patients experienced no complications. Three OG patients and 1 CG patient experienced more than 2 complications (Table 5). Compared to LG patients, the adjusted odds ratio for complications among OG patients was 8.78 (P = 0.001), and the adjusted odds ratio for complications among CG patients was 1.85 (P = 0.316) (Table 6). In addition, multivariate analyses were performed on various factors affecting postoperative complications except operative approach. Age, BMI, diabetes, hypertension, and operation time were not associated with the prevalence of complications (Table 7).
Hartmann operation is frequently used for emergency operations involving the left colon. Among the most important concerns for patients who have undergone a Hartmann procedure is reversal of the colostomy. Reversal of a Hartmann colostomy can be difficult to achieve, owing to unusual abdominal anatomy related to the patientŌĆÖs disease, injury, or surgical history; this is often in the form of multiple adhesions, which increase the tendency for excessive intraoperative bleeding. Therefore, many patients (~40%ŌĆō50%) who have undergone a Hartmann operation are not good candidates for colostomy reversal or may refuse the operation [6]. The reversal rate was 40.5% in our study, which was lower than in other studies (~50%ŌĆō60%) [6]. We believe that age was the most important factor influencing the low reversal rate in our study. The majority of patients who had undergone Hartmann operation and were included our analysis were elderly patients over 70 years old (98 patients, 57.6%); the reversal rate was 33.6% (33 patients) among elderly patients and 48.6% (35 patients) among patients younger than 70 years of age. Younger patients may have been more adamant with expressing their desire for a reversal operation, as they expected longer postoperative survival and a lower rate of postoperative morbidity than elderly patients. On the other hand, many elderly patients refused the reversal operation, similar to what has been reported elsewhere [7].
The duration of hospital stay was significantly shorter among LG patients than OG patients; this was likely associated with the significantly lower morbidity from postoperative ileus or wound-related complications among LG patients. Other studies of laparoscopic vs. open colonic procedures had similar results [6].
Operation time did not vary significantly among the groups. However, the mean operation times in our studyŌĆöboth among LG patients (224.3 ┬▒ 83.5 minutes) and OG patients (222.5 ┬▒ 95.5 minutes)ŌĆöwere longer than in other studies (mean time of 149 minutes) [4, 6-8]. In a review of other similar studies, operation time was the interval between the first skin incision and wound closure whereas the time used in our analysis started at the moment of general anesthesia induction and ended at anesthesia recovery because our retrospective data were collected from anesthesia records. Therefore, the mean operation time in our study was longer than what had been reported previously by similar studies. In our study, the mean LG operation time was longer than the mean OG operation time; even though the difference was not statistically significant, this finding was unexpected. Knowledge of the amount of time required for lysis of adhesions and closure of the laparotomy wound led us to expect that the mean operation time would be longer among OG patients [8].
Hartmann colostomy reversal procedures that are performed later than 6 months after the initial operation are more likely to be associated with postoperative complications, such as ileus, than those with a delay shorter than six months. Other studies have demonstrated that the timing of reversal is important, and 6 months has been proposed as a maximum interval between the initial operation and its reversal [7]. Additionally, anastomosis-related complications are 5 times more frequent in patients with a delay of more than 6 months [7]. The complication rates among OG patients (51.7%) and LG patients (10%) were higher than in previous studies. Studies have generally reported that postoperative complication rates associated with the laparoscopic approach (~15%) are similar to or lower than those associated with open surgery (~30%ŌĆō50%) [6-8].
During the period under study, 39 attempts were made at laparoscopic reversal of Hartmann operation, but only 20 of them (51%) were successful. For 19 patients, laparoscopy was converted to laparotomy. Moreover, six of the 8 patients who had previously undergone a laparoscopic Hartmann operation successfully underwent laparoscopic colostomy reversal. However, only 14 of the 31 patients who had previously undergone an open Hartmann operation successfully underwent laparoscopic colostomy reversal. These results suggest that the probability of a successful laparoscopic colostomy reversal is higher among patients who have previously undergone a laparoscopic Hartmann operation than among those who have previously undergone an open Hartmann operation. However, our analysis revealed that previous operation type did not strongly influence the emergence of complications (P = 0.309). Of note, bleeding during surgery, the length of the remnant rectal stump, and the location of the distal stump did not affect the probability of successful laparoscopic colostomy reversal. Intra-abdominal adhesions were the most common reason for conversion to open reversal, especially when the extensiveness of those adhesions threatened ureteral or vessel injury.
No difference between CG and LG patients in terms of the indication for Hartmann operation was found in this study. The most common indication was colon cancer. This suggests that the extent of resection does not substantially influence the failure or success of laparoscopic colostomy reversal. In this study, the high conversion rate (49%) can be explained in 2 ways. First, when surgery was performed by a less-experienced laparoscopic surgeon, it was often converted to open surgery. Second, conversion was often necessary in single-port laparoscopy cases associated with severe adhesions around the peristomal floor after stoma takedown. Surgical records did not mention the precise degree or location of adhesions, and this can be considered a limitation of our studyŌĆÖs retrospective design; therefore, identifying the reason for conversion in each case with confidence was difficult. Many studies have been done on intra-abdominal adhesions after surgery, and extensive postoperative adhesions have been well established to be more closely associated with laparotomies than with laparoscopic surgery [9, 10]. In the future, research efforts may develop effective antiadhesive agents or strategies, and these would be helpful for colostomy repair surgery [9].
Single-port laparoscopic Hartmann colostomy reversal was performed for only nine patients in our study, but relative to conventional laparoscopic reversal, the procedure was not significantly different in terms of hospital stay or complication rates, owing in part to the small sample size. Elsewhere, single-port laparoscopic Hartmann procedure reversal (18.2%) has been shown to have a lower morbidity rate than open surgery (10%ŌĆō50%) and conventional laparoscopic surgery (14%ŌĆō25%) [11]. We expect that further investigations with prospective comparative studies will be performed.
In conclusion, a laparoscopic Hartmann colostomy reversal is safe and feasible and is associated with superior clinical outcomes, a shorter duration of hospitalization, and fewer postoperative complications, compared to open reversal. When contraindications to laparoscopy are absent, surgeons should favor laparoscopic reversal of HartmannŌĆÖs operation over open reversal.
Table┬Ā1.
Indications for Hartmann operation among patients in the open, conversion, and laparoscopic groups
| Variable |
Reversal of Hartmann colostomy |
No. of cases | P-value | ||
|---|---|---|---|---|---|
| Open group | Conversion group | Laparoscopic group | |||
| Colon cancer | 16 (55.2) | 11 (57.8) | 12 (60) | 39 (57.3) | 0.94a |
| Diverticular perforation | 4 (13.8) | 5 (26.3) | 2 (10) | 11 (16.1) | 0.41b |
| Stercoral colitis | 5 (17.3) | 1 (5.3) | 3 (15) | 9 (13.1) | 0.54b |
| Traumatic colon injury | - | 2 (10.6) | 2 (10) | 4 (6) | - |
| Ischemic colitis | 2 (6.9) | - | 1 (5) | 3 (4.5) | - |
| Postoperative adhesion | 1 (3.4) | - | - | 1 (1.5) | - |
| Sigmoid volvulus | 1 (3.4) | - | - | (1.5) | - |
| Total | 29 | 19 | 20 | 68 | - |
Table┬Ā2.
Clinical characteristics by operative approach
| Variable | Open group | Conversion group | Laparoscopic group | P-valuea |
|---|---|---|---|---|
| Age (yr) | 66.2 ┬▒ 13 | 67.3 ┬▒ 12.4 | 63.7 ┬▒ 12.4 | 0.65 |
| Sex, male : female | 14 : 15 | 10 : 9 | 13 : 7 | 0.51b |
| BMI (kg/m2) | 22.5 ┬▒ 2.8 | 22.9 ┬▒ 2.9 | 23.3 ┬▒ 2.5 | 0.57 |
| Comorbid disease | ||||
| ŌĆāDiabetes | 5 | 6 | 3 | 0.44b |
| ŌĆāHypertension | 13 | 8 | 10 | 0.88b |
| ASA PS classification | 3.1 ┬▒ 2 | 2.84 ┬▒ 1.6 | 2.55 ┬▒ 1.6 | 0.58 |
| Operation time (min) | 222.5 ┬▒ 95.5 | 234.6 ┬▒ 74.7 | 224.3 ┬▒ 83.5 | 0.88 |
Table┬Ā3.
Statistical results for hospital stay in the open, conversion, and laparoscopic groups
| Group | Hospital stay (day) | P-valuea |
|---|---|---|
| Open (n=29) | 16 ┬▒ 9.5 | 0.028 |
| Conversion (n=19) | 13.68 ┬▒ 6.59 | |
| Laparoscopic (n=20) | 10.15 ┬▒ 2.94 |
Table┬Ā4.
Comparison analysis between the open group and the laparoscopic trial group
| Variable | Open group | Laparoscopic trial group (CG + LG) | P-valuea |
|---|---|---|---|
| Age (yr) | 66.2 ┬▒ 13 | 65.4 ┬▒ 12.4 | 0.80 |
| Sex, male : female | 14 : 15 | 23 : 16 | 0.38b |
| Body mass index (kg/m2) | 22.5 ┬▒ 2.8 | 23.1 ┬▒ 2.7 | 0.35 |
| Comorbid disease | |||
| ŌĆāDiabetes | 5 | 9 | 0.55b |
| ŌĆāHypertension | 13 | 18 | 0.91b |
| ASA PS classification | 3.1 ┬▒ 2 | 2.69 ┬▒ 1.6 | 0.37 |
| Operation time (min) | 222.5 ┬▒ 95.5 | 229.3 ┬▒ 78.5 | 0.75 |
| Hospital stay (day) | 16 ┬▒ 9.5 | 11.8 ┬▒ 5.3 | 0.04 |
Table┬Ā5.
Postoperative complications after reversal of Hartmann operation (n = 68)
Table┬Ā6.
Results of the multivariate logistic regression analysis of postoperative complications by operative approach
| Group |
Complications |
P-valuea | Crude OR (95% CI) | P-value | Adjustedb OR (95% CI) | P-valuec | |
|---|---|---|---|---|---|---|---|
| Presence | Absence | ||||||
| Laparoscopic | 2 (10.0) | 1 (90.0) | 0.011 | Reference | Reference | ||
| Conversion | 7 (36.8) | 12 (63.2) | 1.83 (0.56ŌĆō5.99) | 0.314 | 1.85 (0.55ŌĆō6.21) | 0.316 | |
| Open | 15 (51.7) | 14 (48.3) | 9.64 (1.88ŌĆō49.3) | 0.007 | 8.78 (1.69ŌĆō45.55) | 0.010 | |
Table┬Ā7.
Results of the multivariate analysis of postoperative complications by clinical characteristics
| Variable | No. of patients | No. of complications | P-valuea |
|---|---|---|---|
| Age (yr) | 0.74 | ||
| ŌĆāŌēź70 | 33 | 11 | |
| ŌĆā<70 | 35 | 13 | |
| Body mass index (kg/m2) | 0.55 | ||
| ŌĆāŌēź25 | 17 | 5 | |
| ŌĆā<25 | 51 | 19 | |
| Diabetes | 0.54b | ||
| ŌĆāPresent | 14 | 6 | |
| ŌĆāAbsent | 54 | 18 | |
| Hypertension | 0.59 | ||
| ŌĆāPresent | 31 | 12 | |
| ŌĆāAbsent | 37 | 12 | |
| Operation time (min) | 0.20 | ||
| ŌĆāŌēź226 | 27 | 12 | |
| ŌĆā<226c | 41 | 12 |
REFERENCES
1. Hartmann H. Note sur un proc├®d├® nouveau dŌĆÖextirpation des cancers de la partie terminale du c├┤lon. Bull Mem Soc Chir Paris 1923;49:1474ŌĆō7.
2. Cellini C, Deeb AP, Sharma A, Monson JR, Fleming FJ. Association between operative approach and complications in patients undergoing HartmannŌĆÖs reversal. Br J Surg 2013;100:1094ŌĆō9.


3. Maitra RK, Pinkney TD, Mohiuddin MK, Maxwell-Armstrong CA, Williams JP, Acheson AG. Should laparoscopic reversal of HartmannŌĆÖs procedure be the first line approach in all patients? Int J Surg 2013;11:971ŌĆō6.


4. Park JM, Chi KC. Laparoscopic reversal of HartmannŌĆÖs procedure. J Korean Surg Soc 2012;82:256ŌĆō60.



5. Walklett CL, Yeomans NP. A retrospective case note review of laparoscopic versus open reversal of HartmannŌĆÖs procedure. Ann R Coll Surg Engl 2014;96:539ŌĆō42.



6. Ng DC, Guarino S, Yau SL, Fok BK, Cheung HY, Li MK, et al. Laparoscopic reversal of HartmannŌĆÖs procedure: safety and feasibility. Gastroenterol Rep (Oxf) 2013;1:149ŌĆō52.




7. Toro A, Ardiri A, Mannino M, Politi A, Di Stefano A, Aftab Z, et al. Laparoscopic reversal of HartmannŌĆÖs procedure: state of the art 20 years after the first reported case. Gastroenterol Res Pract 2014;2014:530140.




8. Melkonian E, Heine C, Contreras D, Rodriguez M, Opazo P, Silva A, et al. Reversal of the HartmannŌĆÖs procedure: a comparative study of laparoscopic versus open surgery. J Minim Access Surg 2017;13:47ŌĆō50.



9. Diamond MP, Wexner SD, diZereg GS, Korell M, Zmora O, Van Goor H, et al. Adhesion prevention and reduction: current status and future recommendations of a multinational interdisciplinary consensus conference. Surg Innov 2010;17:183ŌĆō8.