INTRODUCTION
A variety of complications is associated with stomas. Skin-related complications, bowel obstructions, stoma retractions and parastomal hernias are frequent in ileosotmies [
1]; parastomal hernias, skin complications and prolapses are frequent complications for colostomies [
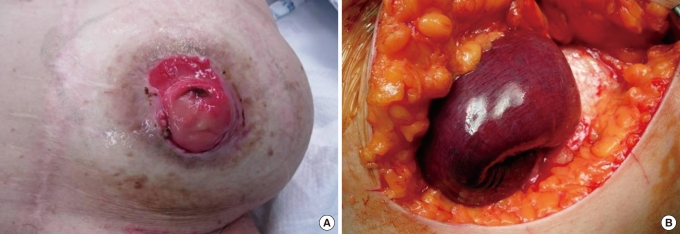
2]. Parastomal hernias develop in 5-30% of stoma patients and cause asymmetries of the abdominal wall and difficulties in applying stoma bags. Even though poor general conditions of some patients prohibit surgical corrections, aggressive treatments are necessary for patients with pain, problems in wearing stoma appliances, prolapses of stomas, necrosis of a herniated bowel and serious cosmetic problems [
3]. Suggested causes of parastomal hernias are postoperative weight gain, increased intra-abdominal pressure combined with weakened abdominal muscles, and old age; other than these, hernias can occur in cases of excessive extension or contraction of a muscle and in cases of improper parastomal anchoring [
4].
Correction of a parastomal hernia is not easy, and high recurrence rates after surgical corrections are reported [
5]. Relocation of the stoma has been known to cause a low recurrence rate in the treatment of parastomal hernias, but recently local correction, including primary closure of the fascial defects with reinforcement by artificial membrane, has been preferred, and prevention of a hernia by using artificial membranes have frequently been tried. In this study, by analyzing the results for the each surgical method, we attempted to find a suitable surgical method for repairing a parastomal hernia.
DISCUSSION
A parastomal hernia is an incisional hernia of the abdominal wall in the site of a stoma [
4]. The incidence of parastomal hernias is not yet known, but most reports say that it is over 30% [
5]; it was reported to be 33% in a prospective study of end colostomy patients [
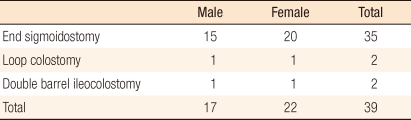
6]. During the period of this study, the incidence of parastomal hernias for the responsible surgeon was 6.6% (19 out of 290 cases): 14.0% (8 out of 57 cases) for the abdominoperineal resection; 6.4% (9 out of 141 cases) for the Hartmann's operation; and 2.2% (2 out of 92 cases) for the loop colostomy. Although there have been numerous studies on and devices for parastomal hernias until now, complete prevention and treatment are not easy to attain.
The frequency of parastomal hernias can vary from report to report, and it can vary with the types and the forms of the stomas. These differences, besides the different incidences themselves, can be attributed to the methods and the criteria used for diagnosis. A parastomal hernia is suspected in patients with subjective symptoms, and it can be diagnosed by physical examination with stoma pouches removed or by radiologic imaging. If the hernia reduces with ease when the patient is in the supine position due to the large defect in the abdominal wall or if the abdominal wall is too fat, a parastomal hernia may be difficult to diagnose through the physician's examination alone. Gurmu et al. [
7] stated that diagnosis of a hernia might depend on the physician and that the result of the physician's examination might be different from that of radiologic imaging. A CT scan may not detect a hernia when the patient is in a supine position. As a solution to this, Janes et al. [
8] mentioned that during a CT scan, the prone position of the patients can help the diagnosis of a parastomal hernia by easily evoking the hernia.
Types of stomas are also a factor in the incidence of parastomal hernias. In cases of end colostomies, incidences of 4-48% are being reported, and in cases of loop colostomies, 0-30.8% are being reported; in the case of the loop colostomy, the low incidence of parastomal hernias is due to its temporary nature, the follow-ups being short and the stoma being taken down before the hernia develops [
4]. This is consistent with the fact that most of the patients in our study were end colostomies with permanent usage. Additionally, in the case of the end colostomy, the mesentery, including feeding vessels, must be a part of the anchoring suture to the abdominal wall. However, in the case of the loop colostomy, most of the part anchored to the abdominal wall is the anti-mesenteric border, which is easy to handle and so flexible that it can be readily anchored to the abdominal wall and can be adaptable to the muscle extension. The lower incidence of parastomal hernias of loop stomas can be attributed to these factors.
The causes of parastomal hernias are divided into patient factors and technical factors. Obesity, malnutrition, increased intra-abdominal pressure, steroids, malignancy, advanced age, and wound infection are referred to as patient factors, but with little evidence [
4]. Meanwhile, Pilgrim et al. [
6] reported in their recently conducted prospective studies that the size of the defect in the abdominal wall and the patient's age were independent contributing factors for parastomal hernias. Parastomal hernias developed in the early years, as in our patients, with the latest development reported being as late as 20 years [
1] and half of the parastomal hernias developing in the first 2 years [
4]. The clustered occurrence of parastomal hernias in the early years may support the importance of technical factors for the development of parastomal hernias.
The treatments for parastomal hernias have traditionally been relocation or suture repair of the fascia [
9]. Although the relocation, contrary to our results, has been reported often as having better short-term results [
3,
9], those studies were not prospectively randomized, so it is rash to jump to a conclusions. Since our study was not a prospective study either, the lower (and comparable to mesh repair) incidence of recurrence in suture repair patients than in relocation patients may be caused by fewer patients of large defects with severe hernias in the suture repair group. The only thing to note is that in the early study period, many reposition surgeries were performed, resulting in many recurrences; after the mesh repair procedure was started, recurrences were fewer (
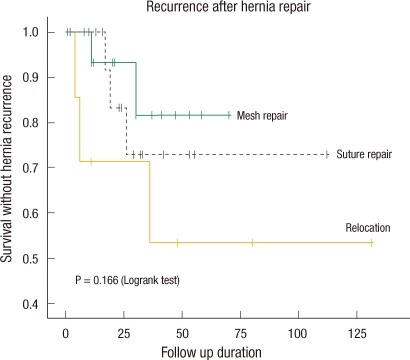
Fig. 5). Although the two surgical methods were not assigned in prospective random fashion, they were separated according to the timing (
Fig. 2), and the suspicion that the patients expected to have low recurrence was artificially incorporated into mesh repair group, can be avoided which supports the reliability of this study. Even though the small number of enrolled patients prevents this result from being statistically significant, it result is consistent with that of other investigators. Now, mesh repair is regarded as the best surgical method for repairing a parastomal hernia [
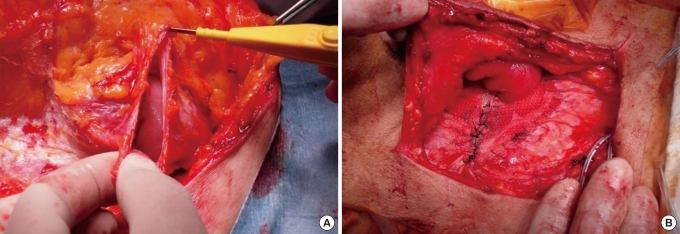
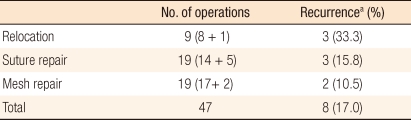
10]. We need further verification of the results with more patients in the future.
There were no cases of emergency surgery in the mesh repair group because perforation or strangulation of the herniated bowel may cause infection of the mesh, which is a very serious complication. The infection rates reported for non-absorbable mesh are not high (4-6%), but these rates are for elective surgery [
11,
12]. Mesh can be used safely in clean-contaminated surgery [
13], but emergency surgery for such as bowel perforations may cause high risk due to contamination with stools or intestinal contents [
10]. Infection or adhesion of the bowel on the mesh applied for the prevention or treatment of a parastomal hernia sometimes causes serious complications, and these are the most important reasons for the hesitation in using mesh in parastomal hernia operations [
14].
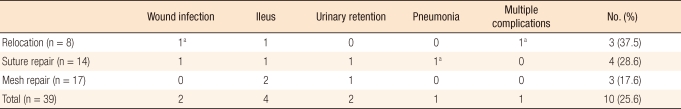
In this study, surgical complications were observed in 3 out of 4 emergency surgery cases (75%), and in 7 out of 35 (20%) elective surgery cases. Among them, one patient who underwent emergency surgery died due to postoperative pneumonia. Emergency surgery is necessary in cases of incarceration, strangulation and possibility of perforation, and the complication rate becomes high in these situations. The larger number of complications in relocation patients is thought to be partly due to the larger number of emergency operations. Excluding the emergency operations, the complication rate for relocation patients of 16.7% (1 of 6 cases) is comparable to that of suture repair (25%, 3 of 12 patients) and to that of mesh repair (17.6%, 3 of 17 cases). Emergency surgery is not thought to elevate the recurrence rate because for each operation method, there were no recurrences in emergency surgery patients. However, because mesh cannot be used in emergency surgery due to the chance of infection, more recurrences may be associated with the operation method rather than the emergency situation per se, which can be addressed with more patients. Also, most results, including our results, were not based on prospective randomized studies, which implies that more patients with good general conditions were in the mesh repair group than in the relocation group. However, the fact that more recurrences did not occur in emergency operations means, paradoxically, that we must not say that the relocation method, which was performed more in patients with poor general condition, has a higher recurrence rate because it was performed on patients with poor general conditions.
The recent focus of parastomal hernias is on the preventive use of meshes and on the development of less-complicated biological materials. Serra-Aracil et al. [
14] mentioned that preventive reinforcement of the fascia by using artificial materials during the initial stoma formation does not make complications higher with prevention of parastomal hernias. Janes et al. [
15] stated, based on the result of a 5-year follow-up of randomized patients, that the superiority of preventive mesh lasted for over 5 years and that neither strictures nor fistulas were associated with the use of mesh. Additionally, Hammond et al. [
16] reported lower complication rates when using collagen implants, which have higher biocompatibility than polypropylene mesh. We hope safer, more concrete, and more convenient methods for preventing parastomal hernias will be devised in the future.
Although we could not attain statistical significance due to the limited number of cases, mesh repair showed lower recurrence and complication rates and shorter hospital stays than relocation among the methods used for parastomal hernia surgery, and these results are consistent with those of others. Prospective randomized studies are necessary if more reliable evidence is to be obtained, especially, for complicated parastomal hernias, such as perforations or strangulations; even more research is needed.