Surgical Outcomes and Risk Factors in Patients Who Underwent Emergency Colorectal Surgery
Article information
Abstract
Purpose
Emergency colorectal surgery has high rates of complications and mortality because of incomplete bowel preparation and bacterial contamination. The authors aimed to evaluate the surgical outcomes and the risk factors for the mortality and the complication rates of patients who underwent emergency surgery to treat colorectal diseases.
Methods
This is a prospective study from January 2014 to April 2016, and the results are based on a retrospective analysis of the clinical results for patients who underwent emergency colorectal surgery at Chosun University Hospital.
Results
A total of 99 patients underwent emergency colorectal surgery during the study period. The most frequent indication of surgery was perforation (75.8%). The causes of disease were colorectal cancer (19.2%), complicated diverticulitis (21.2%), and ischemia (27.2%). There were 27 mortalities (27.3%). The major morbidity was 39.5%. Preoperative hypotension and perioperative blood transfusion were independent risk factors for both morbidity and mortality.
Conclusion
These results revealed that emergency colorectal surgeries are associated with significant morbidity and mortality. Furthermore, the independent risk factors for both morbidity and mortality in such patiients were preoperative hypotension and perioperative transfusion.
INTRODUCTION
Owing to the Westernization of dietary habits and the aging of society, the occurrence rates of malignant colorectal disease and benign diseases such as diverticulitis and intestinal ischemia are increasing in Korea [1]. Colorectal cancer is often diagnosed at an early stage owing to recent improvements in diagnostic methods, such as colonoscopy and abdominal computerized tomography, and the average treatment outcome continues to improve. However, various benign colon diseases are often diagnosed and treated when complications such as perforation and obstruction occur. In such cases, emergency surgery is usually required, and the morbidity and the mortality rates are high due to the performance of the emergency surgery itself, incomplete bowel preparation, bacterial proliferation, and contamination [23].
Several factors, including the patient's age and preoperative condition, complications, and disease type, have been reported to affect the mortality and the morbidity rates [45]. Because most previous studies were retrospective, the authors of the present study conducted a prospectively designed study to examine the mortality and the morbidity rates in patients undergoing emergency surgery to treat various colorectal diseases and to identify potential risk factors for mortality and morbidity.
METHODS
This study was performed by retrospectively reviewing clinical outcomes of prospectively collected information on patients who had undergone emergency colorectal surgery from January 2014 to April 2016. This study was approved by the Institutional Review Board of Chosun University Hospital (approval number: 2013-10-009). Inclusion criteria were cases of emergency surgery caused by primary colorectal diseases. Pediatric patients and patients with appendicitis, trauma, and iatrogenic injury, as well as those undergoing reoperation caused by complication of elective abdominal surgery, were excluded.
The preoperative assessment included sex, age, presence or absence of comorbidities, and hypotension defined as a systolic blood pressure of 90 mmHg. In addition, a survey was conducted by using the American Society of Anesthesiologist (ASA) physical status classification grade, that score being based on the physical condition of the patients undergoing the surgery and anesthesia [6]. Intraoperative observations, such as the indications for surgery, the operating surgeon, and the amount of blood transfused, were recorded and evaluated. After the surgery, complications and deaths that occurred during hospital stay, as well as the length of hospital stay, were recorded. Mortality was defined as death occurring while in the hospital following surgery. The etiology was recorded as colorectal cancer, diverticulitis, ischemia, stercoral or other.
As for complications, major symptoms that might threaten the life of the patient, such as bowel obstruction, pneumonia, sepsis, renal failure, hemorrhage and pulmonary embolism, were recorded. For statistical analysis, PASW Statistics ver. 18.0 (SPSS Inc., Chicago, IL, USA) was used. A univariate analysis was conducted on the patient-related factors and the surgery-related factors, and the relationship between the mortality and the complication rates were evaluated by using the chi-square test. Factors with P-values ≤ 0.05 were selected, and significant factors were identified after a multivariate analysis had been performed using a logistic regression. Those factors with P-values ≤ 0.05 were considered to be statistically significant.
RESULTS
A total of 108 patients underwent emergency colorectal surgery during the study period. Of these individuals, 9 were excluded because they had an indication for emergency surgery due to trauma or iatrogenic colorectal perforation, such as perforation occurring during colonoscopy; finally, 99 were included in the analysis.
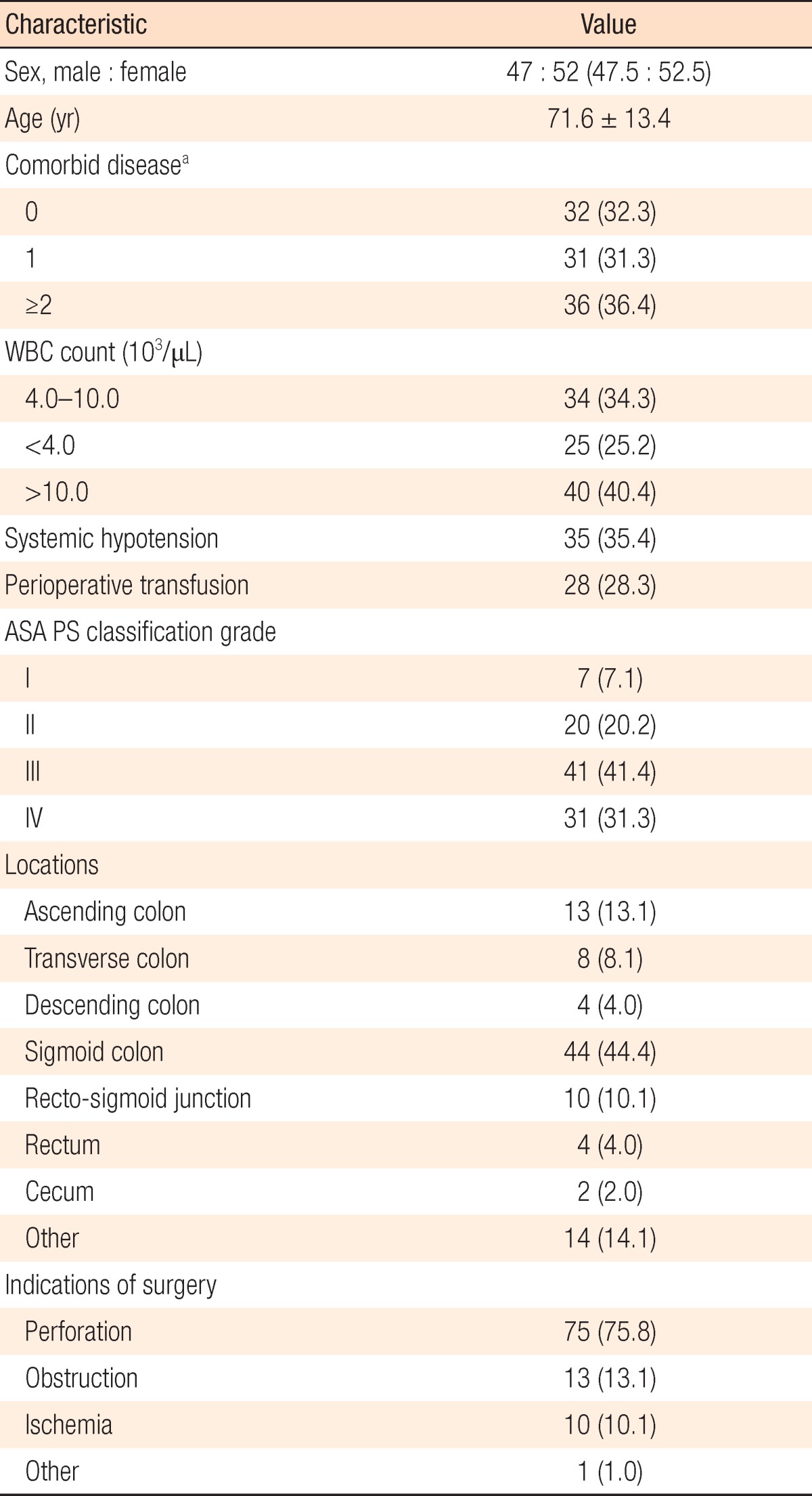
Table 1 shows the included patients' preoperative conditions. The mean age was 71.6 years, and the number of female patients (52.5%) was slightly larger than the number of male patients. Preoperative leukocytosis was found in 40.4% of patients, and leukopenia in 25.2%. Additionally, preoperative hypotension was found in 35.4%, and 28.3% underwent blood transfusion during the perioperative period. According to the ASA physical status classification grade, 72 patients (72.7%) were ranked as grade III or higher. The sigmoid colon was identified as the most common site of the lesion. Furthermore, regarding the indication for surgery, 75 had peritonitis due to perforation, which was the most common of all indications observed in the study's cohort (Table 1).
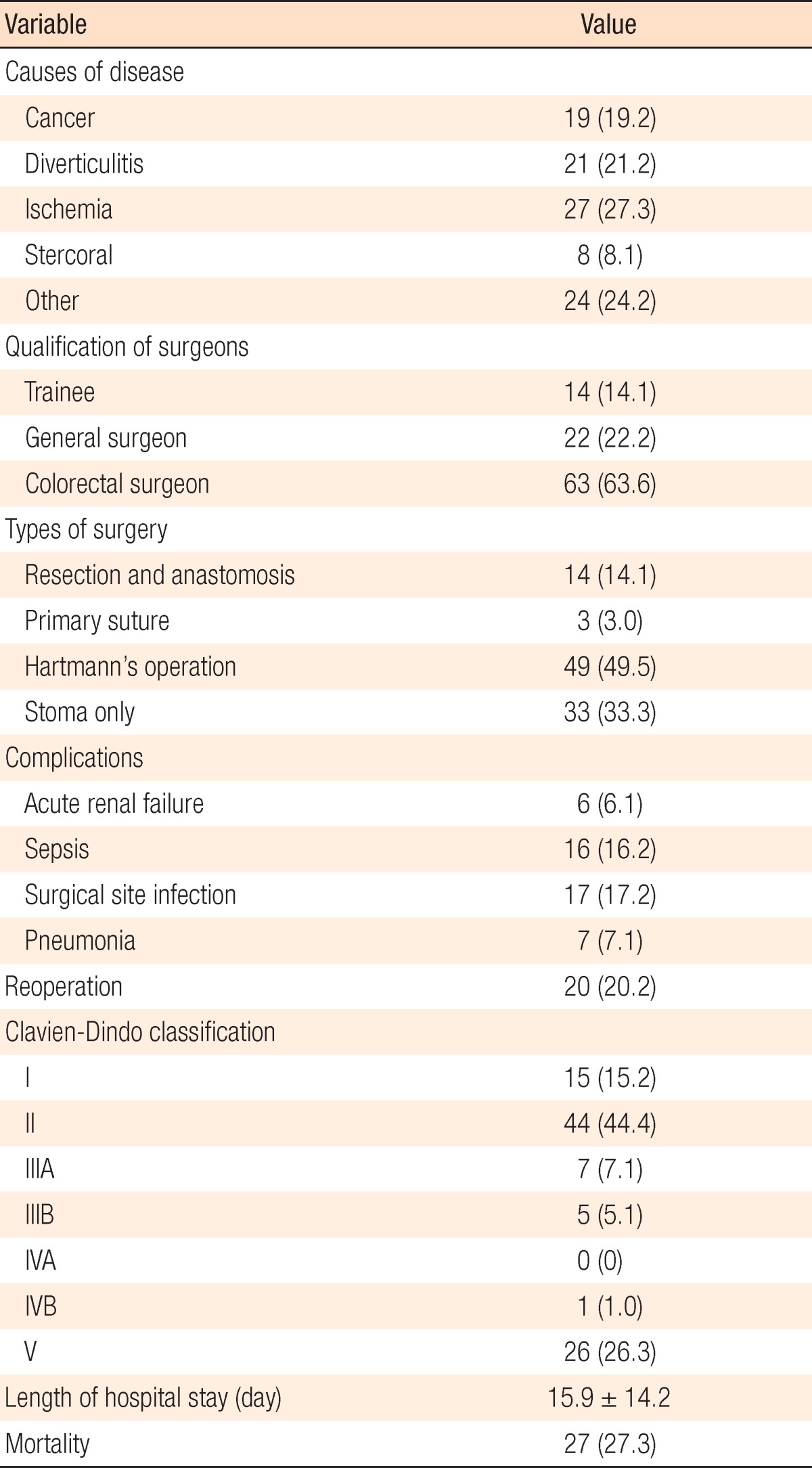
With respect to the cause of disease, 19.2% of the patients had a malignant tumor, 21.2% had diverticulitis, 27.3% had ischemia, and 8.1% had an obstruction due to fecal impaction; specific causes were not identified in as many as 20.2%. Regarding the surgical technique employed, the Hartmann's procedure was the most common and was performed in 49 patients. Regarding major complications affecting the morbidity and the mortality rates, 6 patients required emergency dialysis owing to acute renal failure, and 16 were diagnosed with sepsis. In addition, infection at the surgical site occurred in 17 patients, and pneumonia arose in 7 patients. The patients in this study were classified on the basis of their complications according to the Clavien-Dindo classification [7] scheme, with 15 ranked as grade I, 44 as grade II, 12 as grade III, 1 as grade IV, and 26 as grade V. Notably, Clavien-Dindo classification grades of III or higher were defined as major morbidities, and 39 patients (39.5%) were in this group. Reoperation was required in 20 patients, in most of whom wound dehiscence was the reason for reoperation. The mean length of hospital stay was 15.9 ± 14 days, and 27 patients (27.3%) died in the hospital following the surgery (Table 2).
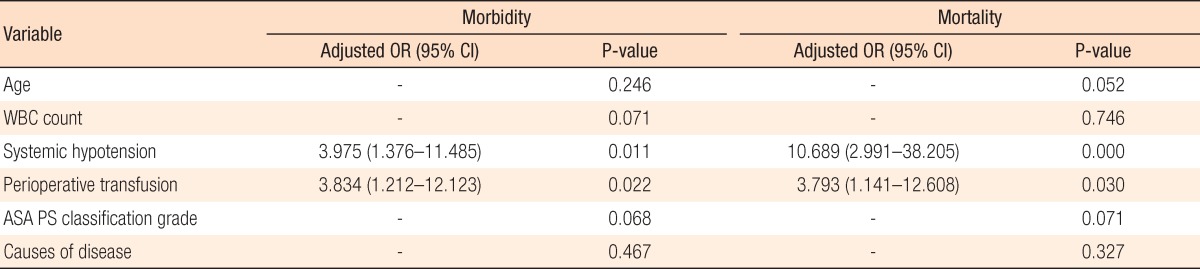
To identify factors related to the mortality and the morbidity rates, we conducted statistical analyses with respect to all variables examined in the study. Patient's age, white blood cell (WBC) count, systemic hypotension, perioperative transfusion, and ASA physical status classification grade were significantly associated with major morbidity. Also, a statistical association with mortality was found with respect to systemic hypotension, perioperative transfusion, and ASA physical status classification grade (Table 3). To predict the risks for mortality and morbidity based on the complex influences of the relevant variables, we conducted a logistic regression test. Systemic hypotension had relative risks of 3.975 and 10.689 for morbidity and mortality, with P-values of 0.011 and 0.000, respectively. Perioperative transfusion had relative risks of 3.834 and 3.793, with P-values of 0.022 and 0.030, respectively. ASA score was associated with mortality rate in grade IV, but not in other grade levels (data not shown). Aside from these, no statistical association was found with regards to any of the following variables: age, WBC count, ASA physical status classification grade, and causes of disease (Table 4).
DISCUSSION
In this prospective study, the mortality rate was 27.3% in patients who had undergone emergency colorectal surgery, and the rate of major morbidity was 39.5%. Additionally, systemic preoperative hypotension and perioperative transfusion were found to be independent risk factors for death and the occurrence of a major morbidity. Moreover, perforation was the most common indication (75.8%) for emergency colorectal surgery, and obstruction was a relatively small indicator (13.1%).
In a population-based study conducted by Kwan et al. [2] in 2008, 54.3% of the patients had a bowel obstruction as their indication for emergency colorectal surgery, and 35.9% had peritonitis. Furthermore, for the cause of disease, a majority of patients had colorectal cancer (63.8%) while diverticular disease was observed to be the most common benign disease. However, in the present study, the rates of colorectal cancer, diverticular disease, and ischemic colitis or colon gangrene were 19.2%, 21.2%, and 27.3%, respectively. Thus, the frequencies of the three major causes of disease were similar, a finding highly inconsistent with previous findings. This inconsistency is considered to be due to recent changes in the treatment paradigm for various colorectal diseases that require emergency surgery. In the case of obstruction due to colorectal cancer, the increased achievement of early cancer diagnoses has reduced the absolute frequency of obstruction. Furthermore, recently, even if an obstruction is diagnosed, in many cases a stent is first inserted to resolve the obstruction, after which elective surgery is performed following an effective bowel preparation [8]. Also, in the case of complicated diverticulitis, a recent trend is increasingly to try nonoperative treatment (e.g., bowel rest and antibiotics) or to perform minimally invasive surgery (e.g., laparoscopic lavage), after which an elective resection is performed later, if necessary, whereas in the past, emergency surgery was performed to treat complicated diverticulitis [910].
Perforation has been reported to occur more frequently because of benign diseases such as diverticulitis than because of a malignant tumor. In addition, perforation due to diverticulitis has been reported to have a relatively favorable prognosis as a peripheral abscess is often formed in such cases and is manifested as localized peritonitis; generalized peritonitis rarely occurs [1011]. Regarding the mechanisms underlying perforation due to colon cancer as the cause of disease, a tumorous area can become perforated directly owing to cancer invasion. Moreover, perforation can occur as an obstruction occurring with tumor progression causes the proximal colon to expand and ischemia to develop. Perforation occurring owing to the expansion of the proximal colon may have a high level of contamination because the feces contains more liquid components in the proximal colon in comparison to the distal colon; thus, the prognosis is reported to be relatively poor [12].
In this study, ischemic colitis or colonic gangrene was the most common cause of disease. Although thrombosis in the inferior mesenteric artery has been reported to be the most common cause of colon ischemia, in most cases, no specific cause is identified [13]. Colon ischemia typically tends to improve naturally after a temporary ischemia attack and does not often progress to peritonitis. However, if gangrene or perforation occurs, then the patient's prognosis is very poor, with a mortality rate of over 50% [13].
The morbidity rate is very high after emergency colorectal surgery and can be as high as 11% to 32%. Age, underlying disease, preoperative hypotension, and/or the cause of perforation have all been suggested as prognostic factors [14]. Also, according to a report, the prognosis can be determined by considering patient factors rather than the time taken for the surgery or the quality of the surgery [14]. The patients in the present study were classified in accordance with the occurrence and the type of morbidity according to the Clavien-Dindo classification scheme [7]. Patients who were grade III or higher were categorized into the major morbidity group, with 39 patients (39.5%) ultimately being placed in this group in this study.
The univariate analysis performed in the present study revealed that age, preoperative WBC count, preoperative hypotension, blood transfusion, ASA physical status classification grade, and lesion location were significant risk factors for major morbidity and that preoperative hypotension, blood transfusion, ASA physical status classification grade, and lesion location were risk factors for mortality. However, in the multivariate analysis, only preoperative hypotension and blood transfusion were identified as independent, significant factors for morbidity and mortality. Like other studies, the present study did not find significant relationships between surgery type or surgery quality and morbidity and mortality. These findings seem to suggest that the patient's condition, rather than the quality of the surgery or the surgical technique, has a greater influence on prognosis.
The simplest indicator of patient condition is patient age. Because emergency colorectal surgery is increasingly being performed more in patients of higher age, a need exists to analyze age-related outcomes. In a study where emergency colorectal surgery was performed in patients aged 65 years or older (mean, 78.1 years), McGillicuddy et al. [15] reported that the mortality rate was 15% and that the rate of major morbidity was 35%; they concluded that high age was a significant risk factor. Another study reported a mortality rate of 28% and a morbidity rate of 81% in Asian octogenarian patients who had undergone emergency colorectal resection and identified ASA physical status classification grade as the only relevant risk factor [16]. In the present study, age, which was coded with 70 years as the cutoff in consideration of the mean patient age (71.6 years), was identified as a risk factor in the univariate analysis, but that correlation was not confirmed in the multivariate analysis. In the multivariate analysis conducted with an age of 80 years as the cutoff, again no correlation of age as a risk factor was found (data not shown).
Interestingly, the mortality rate seemed higher in the present study than in other studies. This is speculated to be due to the high frequency of perforations in the present study whereas obstructions were very common in previous studies. In the present study, the mortality rate was 25.3% among patients with a perforation and was 15.4% among patients with an obstruction, showing a difference between the 2 patient groups.
According to a study by Post et al. [17], intraoperative hypotension is closely associated with the occurrence of morbidities, such as leakage, after colorectal surgery. In the present study as well, the prognosis of patients in whom preoperative hypotension and signs of septic shock were noted was poor. Therefore, preoperative hypotension may be an important factor in the postoperative management of patients. Bernard and colleagues reported that intraoperative transfusion may increase the mortality rate [18]. Although the precise mechanism is unknown, intraoperative transfusion is typically associated with increases in the morbidity and the mortality rates following surgery [19]. Similarly, in the present study, it was identified as the most powerful risk factor. A strong association has been reported between ASA physical status classification grade and the 30-day mortality. ASA physical status classification grades were created in the field of anesthesiology to quantify the physiological condition of patients prior to surgery, but many studies have found that it is also an important predictor of the postsurgery mortality rate [2021]. In the present study, ASA physical status classification grade was significantly correlated with morbidity and mortality in the univariate analysis, but not in the multivariate analysis. In patients whose cause of disease was ischemic or stercoral in nature, rather than cancer or diverticulitis, the morbidity and the mortality rates tended to be higher, although the differences were not statistically significant. This finding is believed to be related most likely to the length of the lesion or the size of the perforation. Additional studies are needed.
A limitation of the present study is small number of patients included. In addition, the diversity in the causes of disease requiring emergency surgery may be a source of statistical bias. This study found the following: emergency colorectal surgery was associated with relatively high morbidity (39.5%) and mortality (27.3%), and the independent risk factors for both morbidity and mortality were preoperative hypotension and perioperative transfusion. Accordingly, in order to improve the outcomes, patients with these risk factors should undergo intensive monitoring and active postoperative management.
ACKNOWLEDGMENTS
This study was supported by a grant from the Medical Research Institute of Chosun University Hospital (2014).
Notes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.