Short-term Outcomes of an Extralevator Abdominoperineal Resection in the Prone Position Compared With a Conventional Abdominoperineal Resection for Advanced Low Rectal Cancer: The Early Experience at a Single Institution
Article information
Abstract
Purpose
This study compared the perioperative and pathologic outcomes between an extralevator abdominoperineal resection (APR) in the prone position and a conventional APR.
Methods
Between September 2011 and March 2014, an extralevator APR in the prone position was performed on 13 patients with rectal cancer and a conventional APR on 26 such patients. Patients' demographics and perioperative and pathologic outcomes were obtained from the colorectal cancer database and electronic medical charts.
Results
Age and preoperative carcinoembryonic antigen (CEA) level were significantly different between the conventional and the extralevator APR in the prone position (median age, 65 years vs. 55 years [P = 0.001]; median preoperative CEA level, 4.94 ng/mL vs. 1.81 ng/mL [P = 0.011]). For perioperative outcomes, 1 (3.8%) intraoperative bowel perforation occurred in the conventional APR group and 2 (15.3%) in the extralevator APR group. In the conventional and extralevator APR groups, 12 (46.2%) and 6 patients (46.2%) had postoperative complications, and 8 (66.7%) and 2 patients (33.4%) had major complications (Clavien-Dindo III/IV), respectively. The circumferential resection margin involvement rate was higher in the extralevator APR group compared with the conventional APR group (3 of 13 [23.1%] vs. 3 of 26 [11.5%]).
Conclusion
The extralevator APR in the prone position for patients with advanced low rectal cancer has no advantages in perioperative and pathologic outcomes over a conventional APR for such patients. However, through early experience with a new surgical technique, we identified various reasons for the lack of favorable outcomes and expect sufficient experience to produce better peri- or postoperative outcomes.
INTRODUCTION
After the introduction of the total mesorectal excision (TME) as the optimal technique for the resection of rectal cancer, oncologic and pathologic outcomes in patients with rectal cancer have significantly improved [1234]. In recent years, anal-sphincter-preserving surgery, in combination with preoperative concurrent chemoradiotherapy (CCRT), has become a common treatment for patients with lower rectal cancer. Traditionally, an abdominoperineal resection (APR) has been regarded as the gold standard for that treatment. Nonetheless, the use of a conventional APR to treat patients with locally advanced low rectal cancer has not improved the oncologic outcomes to the same degree as the use of a low anterior resection (LAR) has [56]. The main reason an APR leads to relatively poor outcomes is the higher rates of a positive circumferential resection margin (CRM) and an intraoperative bowel perforation. Thus, the extralevator APR in the prone position was introduced by Holm et al. [7] to decrease the high likelihood of CRM involvement and perforation.
The extralevator APR in the prone position has oncological and technical advantages. Because the levator muscles are removed along with the anal canal and mesorectum en bloc, a more cylindrical specimen is created, and the amount of tissue removed from around the tumor is sufficient to achieve a free CRM. Also, the perineal dissection allows the creation of sufficient space with better visualization, decreasing the likelihood of dissecting along the wrong surgical plane or perforating the specimen [8]. Perineal dissection in the prone position may help decrease the possibility of intraoperative perforation because it allows the rectum to be prolapsed out after opening the pelvis, giving excellent visualization of the plane between the rectum and adjacent organs [7], even though the position change itself could have a negative effect on the operative field.
There are a variety of opinions on the postoperative and the oncologic outcomes of an extralevator APR. Some contend that the technique has not shown any advantage in terms of oncologic outcomes and is associated with poor postoperative morbidity [910]. Conversely, others contend that an extralevator APR in the prone position has oncologic superiority due to its technical advantages [7811]. Therefore, we aimed to compare the perioperative and the pathologic outcomes of an extralevator APR in the prone position with those of a conventional APR at a single institution. We hypothesized that, compared with a conventional APR, the technical advantages of an extralevator APR in the prone position would translate into acceptable perioperative outcomes and oncologic adequacy.
METHODS
Patients
This was a retrospective study, and informed consent was obtained from all patients before surgery. Between September 2011 and March 2014, an extralevator APR in the prone position was performed on 13 patients with rectal cancer, and a conventional APR in the lithotomy position was carried out on 26 such patients. Eligibility criteria included a pathologically-confirmed rectal adenocarcinoma and patients who had undergone an APR (extralevator or conventional) with a curative intent. At our institution, the indication for using an APR for the treatment of patients with rectal cancer is a tumor that is still invading the anal sphincter muscle in the image finding after preoperative chemoradiotherapy or anal incontinence caused by decreased sphincter function even though the tumor is located at the mid rectum. Especially, when the tumor is located at the level of the anorectal ring or has invaded more deeply adjacent muscles such as the puborectalis muscle and the external sphincter muscle, an extralevator APR, instead of a conventional APR, is recommended for achieving a free CRM. Preoperative evaluations included physical examination, colonoscopy, transrectal ultrasonography, pelvic magnetic resonance imaging, and computed tomography of the abdomen, pelvis, and chest. Except those who refused it, most patients underwent preoperative long-course chemoradiotherapy as part of a multimodality treatment course. The details of the chemotherapy regimens and the radiation treatment schedules are described elsewhere [12].
Study objective
The primary objective was to evaluate the perioperative outcomes of an extralevator APR in the prone position in terms of intraoperative (R0 resection, bowel perforation, pelvic lymph node [LN] dissection, operative time, and intraoperative bleeding) and postoperative (postoperative complication and length of stay) outcomes compared with those of a conventional APR.
The secondary objective was to compare the pathologic outcomes of an extralevator APR in the prone position with those of a conventional APR. The pathologic outcomes included gross and microscopic findings of excised specimens such as tumor size, margin length from tumor, CRM involvement, harvested LNs, lymphovascular invasion, histologic grade, Mandard grade, and pathologic TNM stage (American Joint Committee on Cancer [AJCC] 7th edition).
Surgical procedures for an extralevator APR
All surgeries were performed on the basis of the principles of a TME with autonomic nerve preservation. At the root of the inferior mesenteric artery, either low ligation with principal LN retrieval or high ligation was performed. The rectum was mobilized by sharp dissection, and the visceral pelvic fascia enveloping the mesorectum was separated from the parietal fascia overlying the pelvic cavity under direct vision. Mesorectal excision was performed only as far as the levator muscle was visible; further dissection was not performed. The proximal colon was transected at the level of the pelvic floor, and a sigmoidal stoma was created. For the perineal approach, the patients were rotated and fixed in the prone position. The anus was closed by suturing, and perineal dissection of the anal sphincter was performed halfway between the anal verge and ischial tuberosity to the level where the abdominal procedure was terminated. While keeping the perineal body intact, the levator muscles were sufficiently excised to create a negative CRM. The distinguishing difference between an extralevator and a conventional APR was that a cylindrical specimen, including almost the entire levator muscle, was acquired while performing a more extended perineal dissection.
Pathologic examination
CRM involvement was defined as the presence of tumor cells from the outermost margin of the lesion to the proper mesorectal fascia or a maximum distance between the tumor and the proper rectal fascia of <1 mm. Pathologic analyses were performed by a specialized gastrointestinal pathologist, and the pathologic results were staged according to the 7th AJCC TNM staging system. Tumor regressive changes of the rectal cancer (e.g., residual cancer and fibrosis) in response to chemoradiation were described using the Mandard grading system [13].
Data collection
All information, including the characteristics of the patient and the tumor and the perioperative and pathologic outcomes, were retrospectively collected from the hospital's colorectal cancer database and electronic medical charts. Preoperative carcinoembryonic antigen (CEA) level, tumor location, and history of previous abdominal surgery were included in the characteristics of the patient and the tumor. Data on R0 resection and bowel perforation were recorded in perioperative outcomes. Resection margin, CRM involvement, and pathologic TNM stage (AJCC 7th edition) were recorded in pathologic outcomes.
Statistical analysis
Statistical analyses were performed using IBM SPSS Statistics ver. 20.0 (IBM Co., Armonk, NY, USA). Descriptive data are presented as median and interquartile ranges (IQRs) for continuous variables and as frequencies and percentages for categorical variables. Mann-Whitney U-test was used to analyze continuous variables, and Fisher exact test or linear-by-linear association was used for categorical variables.
RESULTS
Patient and tumor characteristics
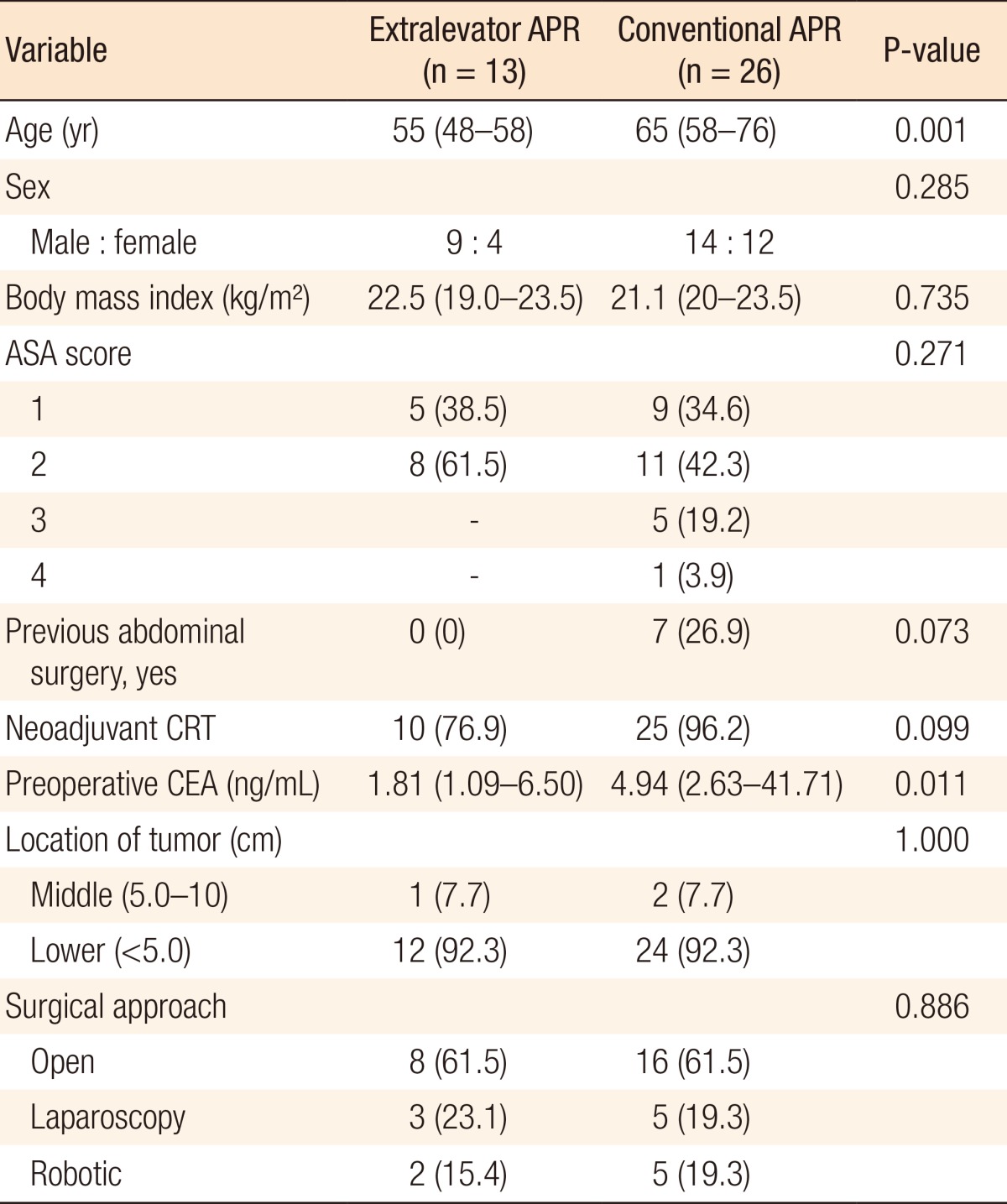
Age and preoperative CEA level were significantly different between the extralevator and the conventional APR groups (median age, 65 years vs. 55 years [P = 0.001]; median preoperative CEA level, 4.94 ng/mL vs. 1.81 ng/mL [P = 0.011]). Only patients in the conventional APR group had a history of previous abdominal surgery (7 of 26, 26.9%). Most patients in both groups were treated with preoperative chemoradiotherapy in accordance with National Comprehensive Cancer Network guidelines for advanced low rectal cancer (10 of 13 [76.9%] vs. 25 of 26 [96.2%], P = 0.099). The sex ratio and distributions of American Society of Anesthesiologists scores were not significantly different between the groups. The distributions of tumor locations and the surgical approaches were also similar (Table 1).
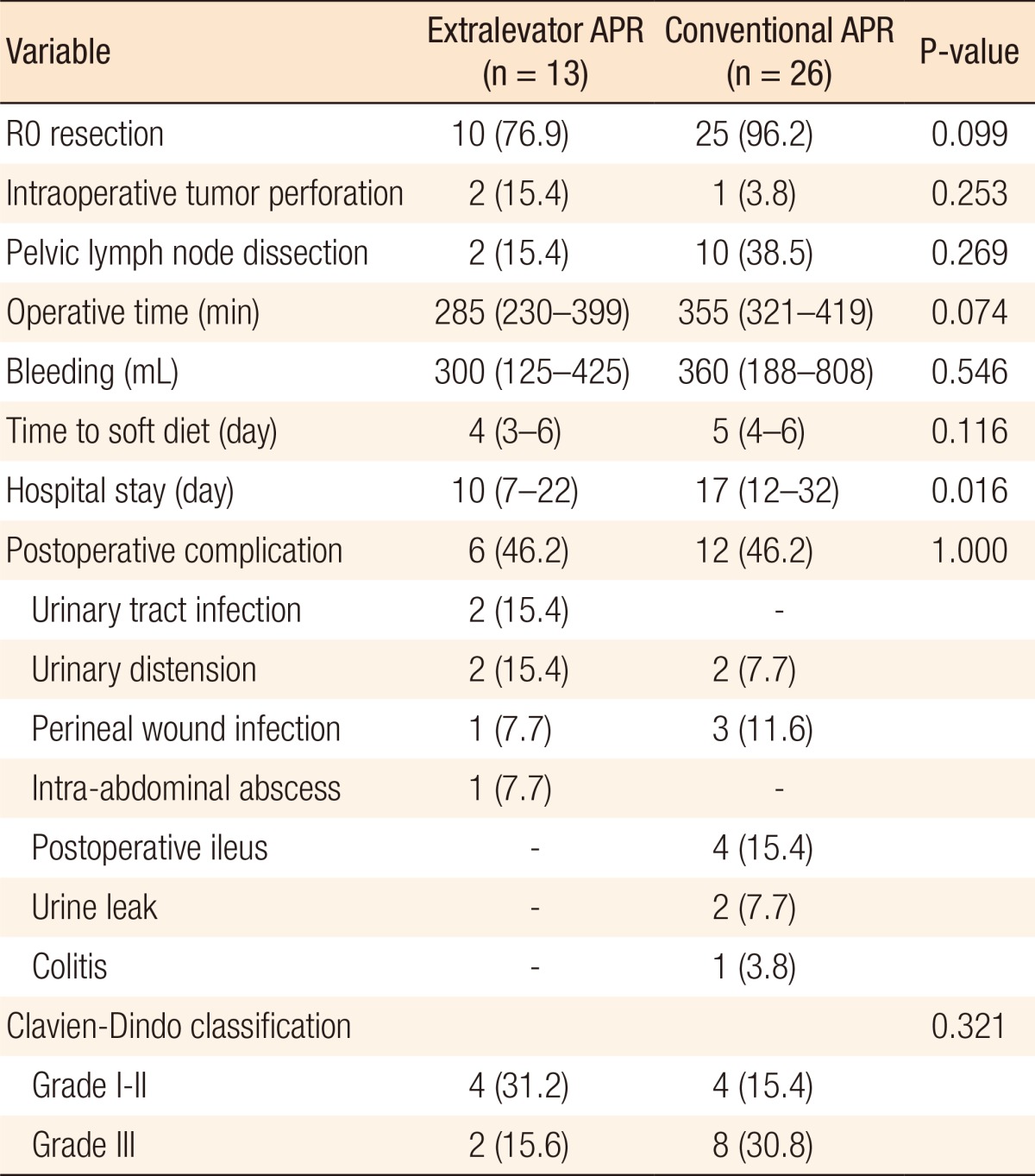
Perioperative outcomes
Intraoperative bowel perforation occurred in 2 patients (15.4%) in the extralevator APR group and 1 patient (3.8%) in the conventional APR (2 of 13 [15.4%] vs. 1 of 26 [3.8%], P = 0.253) (Fig. 1) and except for these patients, all were treated with a R0 resection. The extralevator APR achieved better results than the conventional APR in terms of both operative time and intraoperative bleeding volume (median operative time [IQR]: 285 minutes [230–399 minutes] vs. 355 minutes [321–419 minutes], P = 0.074; median bleeding volume [IQR]: 300 mL [125–425 mL] vs. 360 mL [188–808 mL], P = 0.546). The extralevator APR group started a soft diet after surgery one day earlier than the conventional APR group. The former also had a significantly shorter hospital stay (median hospital stay [IQR]: 10 days [7–22 days] vs. 17 days [12–32 days], P = 0.016). The postoperative complication rates were similar in both groups (6 of 13 [46.2%] and 12 of 26 [46.2%] for extralevator and conventional APR, respectively), but the major complication rate (Clavien-Dindo grade III/IV), such as intestinal obstruction and urine leakage, was greater in the conventional APR group (2 of 13 [15.6%] vs. 8 of 26 [30.8%], P = 0.321) (Table 2).

Bowel perforation induced by both advanced rectal cancer itself and surgical dissection on the tumor site: specimen (A) and tumor site (B).
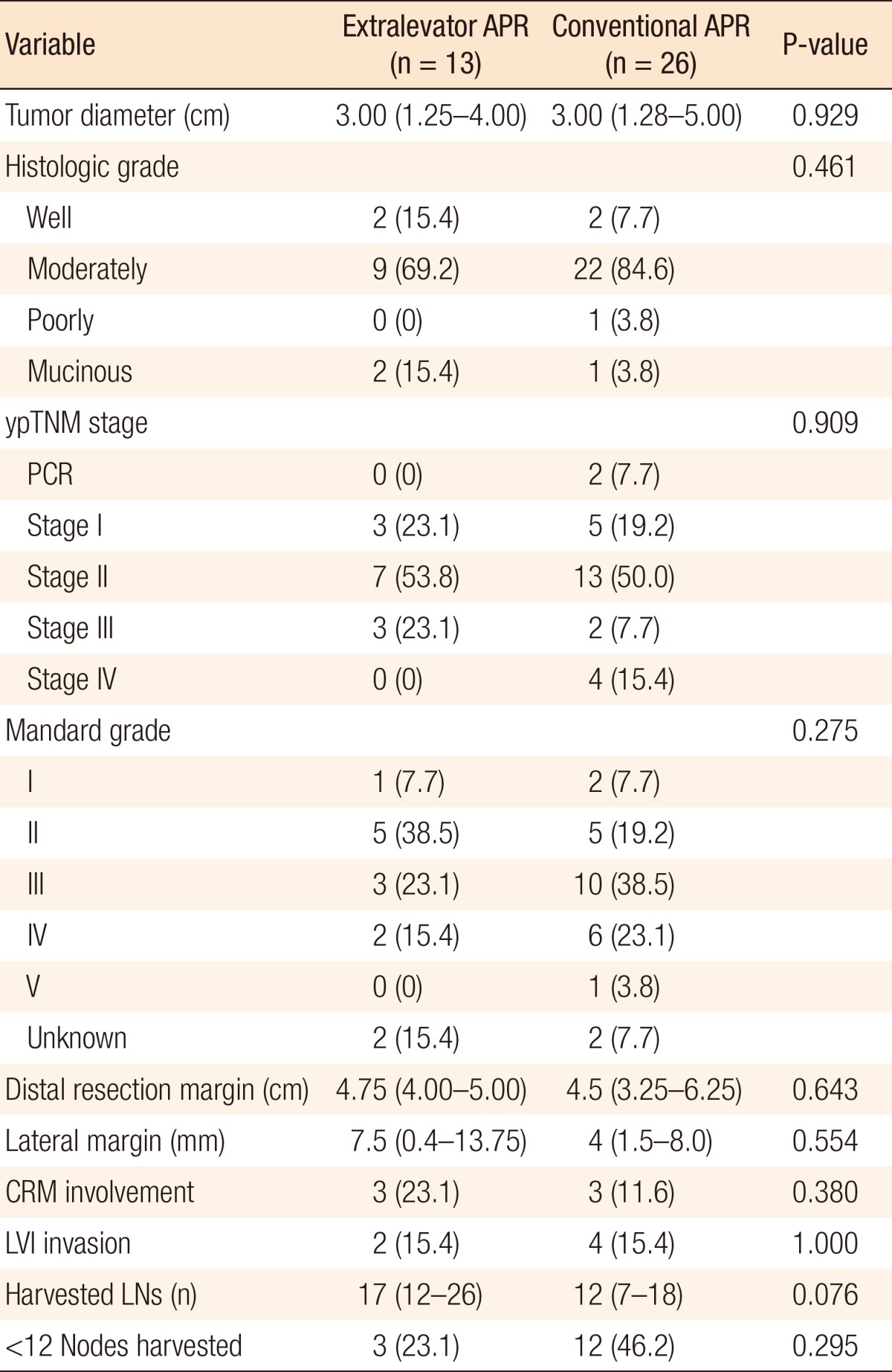
Pathologic outcomes
With regard to pathologic outcomes, both groups had similar results for tumor progression. The most common histologic grade was the moderately differentiated type (extralevator APR group vs. conventional APR group: 9 of 13 [69.2%] vs. 22 of 26 [84.6%], P = 0.461), and stage II was most frequent ypTNM stage (extralevator APR group vs. conventional APR group: 7 of 13 [53.8%] vs. 13 of 26 [50%], P = 0.909). The tumor regression achieved by preoperative chemoradiotherapy was similar in both groups, but the extralevator APR group achieved a slightly better outcome (P = 0.275). Even though no significant differences were noted between the 2 groups, the extralevator APR group acquired a longer lateral margin (median [IQR]: 7.5 mm [0.4–13.75 mm] vs. 4.0 mm [1.5–8.0 mm], P = 0.544), more harvested LNs (median [IQR]: 17 [12–26] vs. 12 [7–18], P = 0.076), and a lower rate of fewer than 12 harvested LNs (3 of 13 [23.1%] vs. 12 of 26 [46.2%], P = 0.295) than the conventional APR group (Fig. 2). The CRM involvement rate was higher in the extralevator APR group compared with the conventional APR (3 of 13 [23.1%] vs. 3 of 26 [11.5%], P = 0.380) (Table 3).

Surgical specimens according to operative method. (A) In the extralevator abdominoperineal resection, the levator muscle was left attached to the mesorectum, which created a cylindrical specimen. (B) In the conventional abdominoperineal resection, a waist was created on the specimen.
DISCUSSION
Our results show that an extralevator APR in the prone position is feasible and that, compared with a conventional APR, the perioperative and pathologic outcomes were acceptable. The median operation time in the extralevator APR group was similar to that reported at other institutions [1014], but the median operation time was shorter than that for conventional APR in our early experience despite the extra position rotation time. Also, the median intraoperative bleeding volume was less in the extralevator APR group. These results were affected by various factors such as the tumor's characteristics (adjacent organ invasion) and the surgeon's view of the operative field during pelvic dissection. Other studies also reported that an APR in the prone position resulted in a shorter operation time and less blood loss due to excellent exposure of the operative field [1516]. An extralevator APR in the prone position is associated with a low tumor perforation rate compared to a conventional APR (tumor perforation rate: 8.2% vs. 28.2, P < 0.001) [14] because it provides surgeons with a better pelvic structure visualization [17]. However, in our early experience, the rate of intraoperative tumor perforation was higher for an extralevator APR than it was for a conventional APR. After reviewing cases with intraoperative tumor perforation, we observed that the rotated operative field, which was not familiar to the surgeon, played an important role in intraoperative tumor perforation, even though advanced tumors also affected that outcome. The prone position during the perineal phase provided a wider and better operative field; nevertheless, surgeons with limited experience with an APR in the prone position encountered difficulty during the perineal dissection because achieving the correct surgical plane in an upside-down operative field, especially when bulky tumors break the surgical plane, was difficult. De Campos-Lobato et al. [18] demonstrated that prone or lithotomy positioning during the perineal phase of an extralevator APR did not affect perioperative morbidity or oncologic outcomes such as tumor perforation, CRM involvement, survival, or recurrence. The authors pointed out that if it is possible to successfully transect the levator muscle through a transabdominal approach, the surgeon has no need to change patient's position. Indeed, Chi et al. [19] and Zhang et al. [20] described a transabdominal levator transection via a laparoscopic approach and argued that an extralevator APR was feasible without position change. We plan to identify which position, prone or lithotomy, is more convenient for surgeons during the perineal phase and adapt it while continuously enhancing our experience with the extralevator APR.
The present study did include some postoperative complicated cases that required reoperation under general anesthesia (Clavien-Dindo class IIIb), including perineal wound infection resulting in dehiscence, urine leakage caused by intraoperative injury, and intestinal obstruction. An increased risk of perineal wound infection, resulting in increased morbidity, has been considered the main disadvantage of an extralevator APR [914]. The rate of perineal wound complication has been reported to range from 35% to 66%, and radiotherapy has been reported to be a significant risk factor [9212223]. Besides, larger perineal wounds (Fig. 3) have been reported to increase the possibility of wound infection. Therefore, surgeons have used a myocutaneous flap technique to close a large perineal defect to reduce the possibility of wound infection, [72425]. We did not initially perform a flap reconstruction to close large perineal defects. To approximate a large defect wound without tension, we first designed the perineal incision line, considering tension-free wound closure, by approximating the bilateral perineal skin; then, we closed the wound layer by layer. The benefits of perineal reconstruction remain to be demonstrated, and we should identify the optimal perineal wound closure method while continuing to increase our experience with the extralevator APR. In the urinary leakage cases, all tumors had penetrated the mesorectal fascia and were positioned at least in the anterior area of the rectum. As a result, the prostate and the urinary tract were partially excised to achieve an R0 resection, and urinary leakage occurred despite surgical reconstruction. The reason for intestinal obstructions that required reoperation was a perineal hernia in all cases. This is a rare complication, but it can occur because APR surgery creates an empty space in the pelvic floor [26]. Moreover, it has been suggested that laparoscopic-assisted APR may contribute to an increase in perineal hernia formation, possibly because of the production of fewer adhesions [2728]. After reviewing the operative record of the cases complicated by intestinal obstructions, we determined that these surgeries were performed with a laparoscopic or robotic approach. We found that although an extralevator APR created a large perineal defect, it did not cause intestinal obstruction or perineal hernia; this is in contrast with another study that described an increased rate of perineal hernias for an extralevator APR compared to a conventional APR [29]. We have recently endeavored to reduce the perineal-hernia rate with the use of a mesh fixation on the pelvic inlet or an omental patch positioned in the pelvis; the results will be determined after collecting further data on postoperative complications following an APR. The length of hospital stay was most strongly influenced by the severity of the postoperative complication, and the median length was longer for the conventional APR group compared both to the extralevator APR group and to values published previously [911]. The median length of hospital stay in the extralevator APR group was similar to those reported in earlier studies regardless of the method of approach [11143031]. Consequently, we can conclude that the rate of severe postoperative complications and the longer hospital stay were not caused by the surgical technique (extralevator or conventional), but rather were due to tumor's characteristics or the method of approach.
One study comparing extralevator and conventional APRs reported a relatively lower local recurrence rate in the extralevator APR group (5-year local recurrence rate: 5% vs. 23%, P = 0.03) [32]. They concluded that this was attributable to the effort to increase the amount of resected specimen containing the anal canal, levators, and complete mesorectum. With regard to the pathologic outcomes of previous studies, the CRM involvement rate varied from 14.8% to 27.6% with the extralevator resection technique [81432], and these results were favorable compared with those for a conventional APR [33]. Conversely, a recent, prospective, large-volume study found that the extralevator technique and tumor stage could be risk factors affecting CRM involvement. However, the study had several limitations including selection bias, patients in the extralevator group being more likely to have received neoadjuvant chemoradiation therapy, and a tendency toward a higher tumor stage in the extralevator group [34]. In our study, the CRM involvement rate was higher in the extralevator APR group. In the cases involving CRM, the tumor was aggravated with invasion of the mesorectal fascia or adjacent organs. Increasing tumor stage and fixed tumor have previously been shown to increase the risk of CRM involvement [3536]. Tumor characteristics, including increased T-stage and postradiation fibrotic change, as well as inexperience with the extralevator APR technique, might play an important role in CRM involvement. Even though the amount of tissue removed around the tumor was increased by using the extralevator plane, locally advanced tumors that did not regress after CCRT were difficult to excise completely. In addition, fibrotic tumor changes after CCRT made the tumor margin unclear, and a microscopic residual tumor remained among the fibrotic tissue, even though the surgeon had grossly confirmed a radial free margin intraoperatively.
CCRT is now a well-established treatment for patients with locally advanced lower rectal cancer and is associated with a favorable oncologic outcome. As APRs were performed in patients with advanced lower rectal cancer, most had undergone preoperative CCRT. According to the Mandard grade (tumor regression grade), which could reflect the effect of CCRT, the extralevator APR group had slightly better results than the conventional APR group. Even though we did not analyze long-term oncologic outcomes, we expect the improved Mandard grade to influence long-term oncologic outcome because it predicts long-term outcome following preoperative chemoradiation therapy in patients with locally advanced rectal cancer [373839].
This study has some limitations. First, it included a relatively small number of subjects and used a nonparametric comparative design. Therefore, the evaluation of statistically significant differences between the 2 groups was restricted. Second, this was an early analysis at a single institution, and the data were collected retrospectively. Third, we did not assess the long-term outcomes, including oncologic results. Despite these shortcomings, this is the first study to compare an extralevator APR in the prone position with a conventional APR in the lithotomy position in Korea. Moreover, we showed various short-term results after an extralevator APR, which is not commonly performed in this country.
In conclusion, compared with a conventional APR, we did not acquire better perioperative and pathologic outcomes by performing an extralevator APR in the prone position for patients with advanced low rectal cancer. For several reasons, these results were different from those in previous studies. First, we did not have enough experience to adapt a new surgical technique of performing a radical excision according to the extralevator plane. Second, after changing the patients to the prone position, the surgeons had to perform the perineal procedure in an unfamiliar position and occasionally had difficulty orienting themselves in the surgical field. Third, advanced tumor invasion into adjacent organs affected the results because it made resection of a sufficient specimen without tumor perforation difficult. We expect better perioperative or postoperative outcomes to be achieved after sufficient experience with the procedure. Further large cohort studies should be carried out to verify the oncologic benefit and safety of the extralevator APR in the prone position before its widespread implementation.
Notes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.