Safety of Nonoperative Management After Acute Diverticulitis
Article information
Abstract
Purpose
The role of surgery in the management of diverticular disease after an episode of acute diverticulitis (AD) managed in a conservative form is evolving. Age, number of episodes of AD, type of episode, and symptoms after the episodes are factors related to the need for elective surgery. The aim of this study is to evaluate the safety of conservative management and the risk factors for emergency surgery after a first episode of AD managed without surgery.
Methods
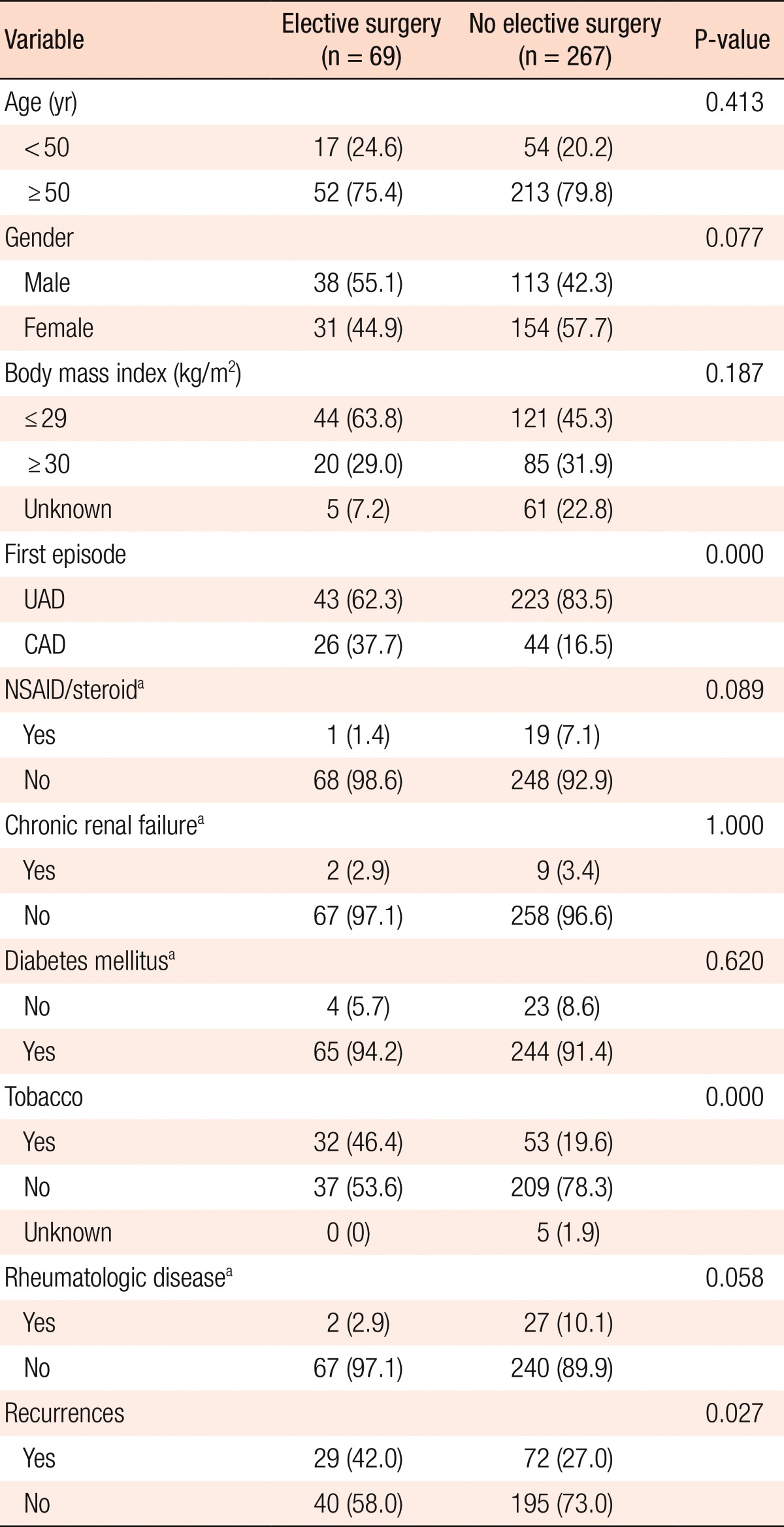
We retrospectively evaluated 405 patients diagnosed as having had a first episode of AD. Sixty-nine patients underwent emergency surgery on the first admission, and 69 patients had an elective operation in the follow-up (group A). The remaining 267 patients were managed initially without surgery (group B). Thirteen of these 267 patients needed a further urgent surgical procedure. Factors involved in the decision of elective surgery and the probability of emergency surgery after the first episode of AD managed without surgery were evaluated in relation to demographic factors, risk factors, presence of recurrences, and type of the first episode.
Results
Patients, mean age was 62.7 years, 71 were aged less than 51, and 151 were males. The mean follow-up for patients with nonoperative management was 91.2 months. An elective operation was performed in 69 patients. Compared to patients in group B, those in group A more frequently had a first episode of complicated acute diverticulitis (CAD) (37.1% vs. 16.4%; P = 0.000) and were more likely to be smokers (46.3% vs. 19.3%; P = 0.000) and to suffer more than one episode of AD (42% vs. 26.9%; P = 0.027). Nonoperative management was chosen for 267 patients, but 13 patients needed an emergency operation later. In the multivariate analysis, we found a significant relation between the presence of CAD in the first episode and the need for emergency surgery. There were no differences in surgical mortality between the patients in the two groups, but patients treated with elective surgery had a higher rate of stoma than patients treated non-operatively (7.2% vs. 1.4%; P = 0.028); this difference was not observed in the subgroup of patients with CAD (15.3% vs. 6.8%; P = 0.458).
Conclusion
After an episode of AD, nonoperative management is safe because fewer than 5% of patients will need an emergent procedure in a subsequent attack of AD. A first episode of CAD is the only risk factor for emergency surgery in patients managed conservatively.
INTRODUCTION
Diverticular disease is a common disorder of the colon in the developed world [1]. Many patients with diverticulosis remain asymptomatic, but acute diverticulitis (AD) is one of the commonest complications. Patients who have developed a first episode of AD can remain asymptomatic for life, but are at risk of a new episode of AD, with some of them needing emergency surgery due to complicated acute diverticulitis (CAD). In recent years, the indications for surgery after an episode of AD have been becoming more and more restrictive. Thus, the aim of this study is to evaluate the safety of conservative management and the risk factors for emergency surgery after a first episode of AD that was managed conservatively.
METHODS
The medical records of patients who had been admitted to institution (Department of Surgery, Complejo Hospitalario de Navarra, Pamplona, Spain) and discharged with a diagnosis of AD from 1 January 1999 to 31 December of 2011 were reviewed. Patients were included in the study if they had a clinical and radiological diagnosis of left-sided AD on computed tomography (CT) or ultrasonography and a posterior confirmation of diverticula with an x-ray contrast enema or colonoscopy. If a colon cancer or inflammatory bowel disease was found or diverticula were not demonstrated, patients were not considered for the study.
A surgical procedure was considered urgent if it was performed after an urgent admission and before discharge. In other cases, the procedure was considered elective. Conservative management is referred to patients in whom an elective surgical procedure was not proposed after a first attack of AD.
Age, gender, risk factors, such as smoking tobacco, chronic renal failure (CRF), nonsteroidal anti-inflammatory drugs (NSAIDs) or corticosteroid use, diabetes mellitus (DM), immunodeficiency, body mass index (BMI), type of AD in the first episode (uncomplicated acute diverticulitis [UAD] or CAD), presence of subsequent episodes of AD, posterior elective or urgent surgery, type and mortality of surgery, were recorded for all patients. Patients were divided by BMI into groups of less than or equal to 30 kg/m2 and greater than 30 kg/m2 and by age into groups of less than or equal to 50 years and greater than 50 years based on the results of previous studies. Complicated diverticulitis was defined as AD followed by colonic perforation, abscess, intestinal obstruction, stricture, or fistula. A recurrent episode was defined based on a need for a patient to be admitted to the hospital due to AD or on the evaluation in the Emergency Department. Major morbidity was defined as a complication with grade 3 to 5 in Clavien-Dindo classification.
With respect to the indications for elective surgery, we considered the preponderant motive for surgery though more than one motive might be present in a patient (e.g., a patient could suffer recurrent attacks and persistent symptoms). CAD, as an indication for elective surgery, is noted for patients in whom surgery was indicated after recovery from an episode of CAD. A phone interview or mail questionnaire was done to rule out surgery or admission to any other hospital.
The total number of patients evaluated after a first episode of AD was 405:139 (34.3%) had an episode of CAD, and 266 had an episode of UAD. Sixty-nine patients with CAD underwent an emergency operation during the first admission and were excluded from the study. Thus, the analysis was involved 336 patients. Of these 336 patients, 266 (79.2%) were classified as having UAD and 70 (20.7%) as having CAD. Also, of these 336 patients, 69 underwent elective surgery (group A), and 267 patients were managed conservatively (group B). Patients in group B were treated with dietary modifications and oral or intravenous broad-spectrum antibiotics +/- percutaneous drainage. Metronidazole (1.5 g/24 hours) plus Cefotaxime (1 g/8 hours) is the standard first-line treatment in our institution. Thirteen of the 267 patients who were treated conservatively needed further emergency surgery.
The decision to perform elective surgery and the assessment of the risk of emergency surgery after the first episode of AD that had been managed without surgery were evaluated in terms of demographic factors, risk factors, presence of recurrences, and type of the first episode (UAD or CAD). The study was approved by the research Ethics Committee of the Complejo Hospitalario de Navarra, Pamplona.
Categorical variables were compared using the chi-square test and Fisher exact test when appropriate. A univariate binary logistic regression analysis was used to evaluate the risk of emergency surgery. Independent significant predictors from the univariate analysis were further evaluated by using a multivariable logistic regression analysis model and SPSS ver. 17.0 (SPSS Inc., Chicago, IL, USA). Statistical significance was defined as P ≤ 0.05.
RESULTS
The mean age was 62.7 years (range, 25 to 96 years), 71 (21%) were aged less than 51 years at first admission, and 151 (44.8%) were males. The mean follow-up for patients managed conservatively 91.2 months.
The flowchart in Fig. 1 shows the evolution of patients after a first diagnosis of AD. An elective surgery was performed in 69 patients: 43 cases after an episode of UAD and 26 after an episode of CAD (group A). Twenty-nine patients suffered more than one episode of AD; 59 were classified as Hinchey I and 10 as Hinchey II. A conservative management was chosen for 267 patients (group B). These patients were treated with oral or intravenous broad-spectrum antibiotics; six patients needed percutaneous drainage of abscesses. The characteristics of the patients in both groups are shown in Table 1.
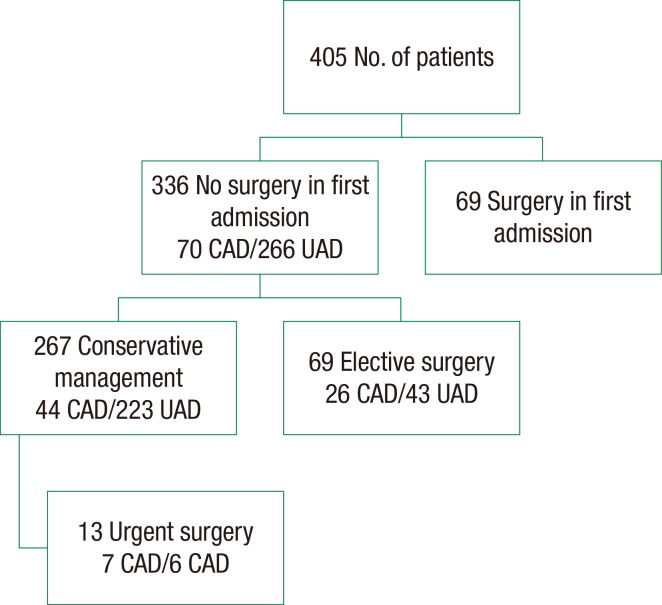
Evolution of the patients after a first diagnosis of acute diverticulitis. CAD, complicated acute diverticulitis; UAD, uncomplicated acute diverticulitis.
The reasons for elective surgery were recurrent attacks in 30 patients (43.4%), persistent symptoms in 27 (39.1%), appearance of fistulae in 6 (8.7%), and CAD in 6 (8.7%). Compared to patients in group B, those in group A had a high rate CAD in the first episode (37.1% vs. 16.4%, P = 0.000), were smokers (46.3% vs. 19.3%, P = 0.000) and had suffered more than one episode of AD (41.4% vs. 17%, P = 0.027). There were no differences regarding BMI, use of NSAIDs or corticosteroids, DM, CRF or immunodeficiency between the two groups.
After elective surgery, one patient died (1.4%), nine patients suffered a major morbidity (12.8%), and five stomas were created (7.1%) (1 colostomy and 4 loop ileostomies). Of the 267 patients in group B, 13 (4.8%) underwent an emergency operation during follow-up due to peritonitis (5 cases), intestinal obstruction (4 cases), abscess (3 cases) and failure of medical treatment (1 case). Four stomas were created (1.4%) (4 colostomies), major morbidity was evidenced in 3 cases (1.1%), and death occurred in 1 case (0.3%). There were no differences in surgical mortality (1.3% vs. 0.3%, P = 0.379) between the two groups, but patients in group A had a higher rate of stoma creation (7.1% vs. 1.4%, P = 0.028) and morbidity (12.8% vs. 1.1%, P = 0.000) than the patients in group B.
In the subgroup of patients with a first episode of CAD, 26 patients underwent an elective procedure, and 44 received nonoperative management. After the elective procedure, no deaths were reported, 4 patients (15.3%) had a major morbidity, and 4 stomas were created. After nonoperative management, 7 patients needed an emergent surgical procedure, and 1 patient died (2.2%), 2 patients suffered a major morbidity (4.5%), and 3 stomas were created (6.8%). There were no differences in the mortality, morbidity or stoma-creation rates between the two groups (Table 2).

Comparison of rates of stoma creation, morbidity and mortality between patients treated with elective surgery and patients with nonoperative management
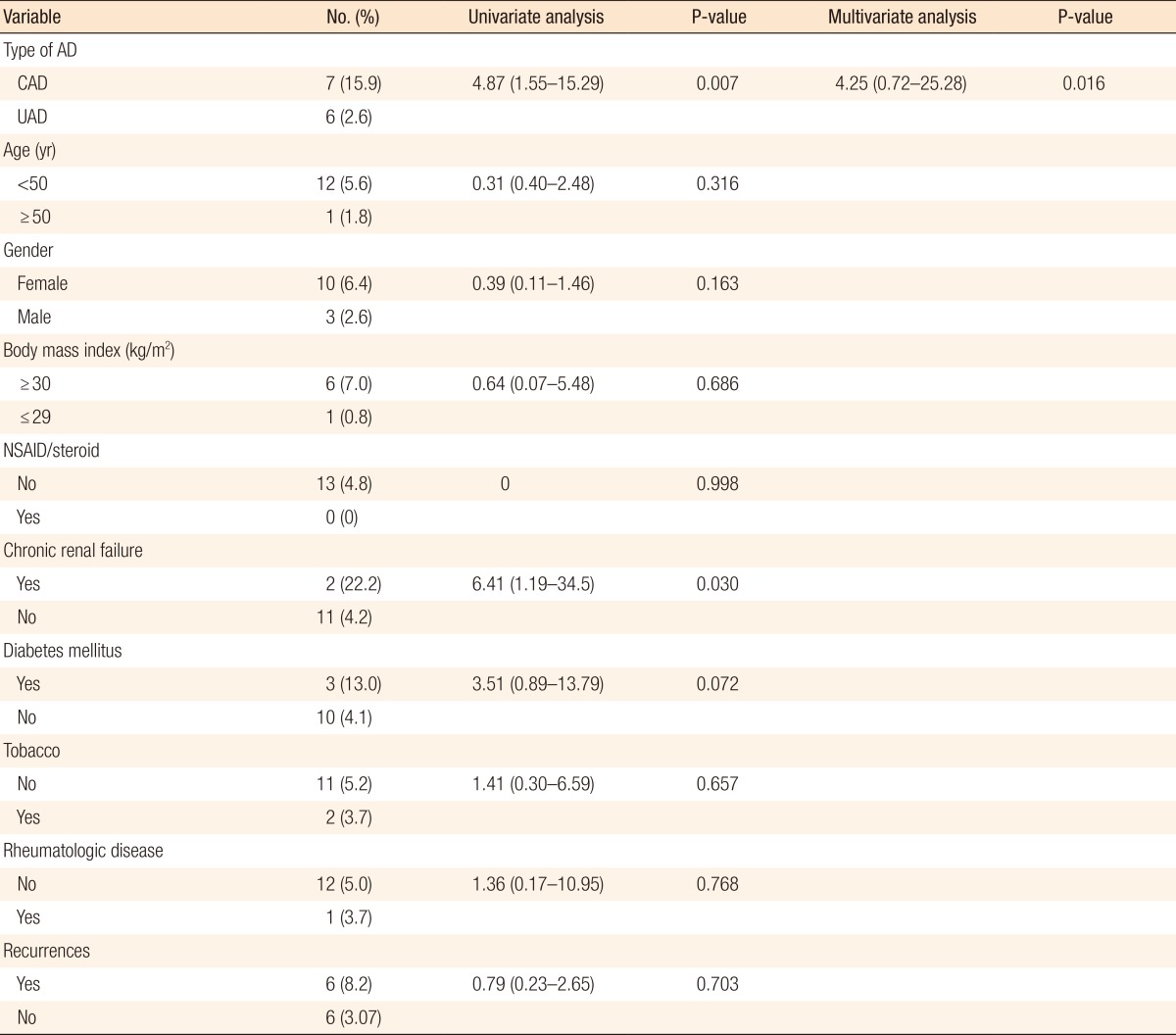
Regarding the 13 patients who had emergency surgery, in the univariate analysis, we found a statistically significant relation between the need for emergency surgery after a first episode of AD managed without elective surgery and (1) the presence of CRF (odds ratio [OR], 6.41; 95% confidence interval [CI], 1.19-34.5; P = 0.030) and (2) the type of the first episode of AD (OR, 4.87; 95% CI, 1.55-15.2; P = 0.007). In the multivariate analysis, only the type of the first episode remained significant (Table 3).
DISCUSSION
Diverticular disease is a common disorder in Western countries. Although the majority of patients with colonic diverticula remain asymptomatic, episodes of AD have been reported in 10%-25% of patients [1, 2]. On the basis of CT findings, Ambrosetti et al. [3] classified AD as moderate diverticulitis and as severe diverticulitis when an abscess, free extraluminal gas, or contrast extravasation was found. In our study, the presence of colonic perforation, abscess, intestinal obstruction, stricture, or fistula was considered as CAD. In our experience, 34.2% of patients suffered a first episode of CAD, which is in agreement with previous reports; in a retrospective analysis of over 502 patients, Eglinton et al. [4] found that 32.8% of the patients had suffered a first episode of CAD.
Natural history of AD is unclear, and the role of prophylactic surgery following a conservatively managed episode of AD is controversial. Prevention of recurrent acute episodes and the need for urgent surgery are some of the main reasons for elective surgery following AD. Morbidity associated with elective surgery and the possibility of recurrence of AD following elective surgery should also be considered.
Elective surgery
In our study, 69 of 336 patients (20.5%) managed without surgery in the first episode of AD, 43 following an episode of UAD (16.4%), and 26 after CAD (37.1%) underwent posterior elective surgery. Dharmarajan et al. [5] reported very similar data: 48% of elective resections after an aggressive protocol of conservative management of CAD.
In recent years, the indications for elective surgery after a first episode of AD managed without surgery are becoming more and more restrictive. For example, the American Society of Colon & Rectal Surgeons, as published by Rafferty et al. [6] in 2006, recommend an elective sigmoid colectomy after recovery from AD based on the individual patient's condition (age, general medical condition, number and severity of attacks, and persistence of symptoms), rather than on the number of attacks of UAD as an overriding factor in the decision to perform surgery. Nevertheless, in our study, elective surgery was indicated more frequently in patients with recurrent attacks (42% vs. 26.9%; P = 0.018). This result may have been influenced by practice parameters that recommend elective resection after two episodes of diverticulitis to reduce morbidity and mortality [7]. The presence of persistent symptoms was the other preponderant indication for elective surgery.
The need for an elective colectomy after recovery from AD in patients younger than 50 years of age remains controversial. Because of their longer life span, these patients have a higher cumulative risk of recurrent attacks. Some reports show a higher rate of complications among young patients compared to older patients [8], but Guzzo and Hyman [9] found only a 0.5% rate of subsequent diverticular perforation in medically-managed young patients with sigmoid diverticulitis. In a recent analysis, patients 45 years of age or younger had not differences in cumulative recurrence of DA compared to patients 46-70 years of age and to patients older than 70 years of age [10]. In our study, younger patients did not have a higher rate of elective surgery.
An elective colectomy has been generally performed after an episode of CAD managed nonoperatively. Kaiser et al. [11] found a 13% recurrence rate for mild cases compared to 41.2% for patients with a pelvic abscess that had been treated conservatively, and Hall et al. [12] showed that patients with a retroperitoneal abscess were at higher risk for recurrent disease. In our experience, a higher rate of CAD was present in group A than in group B (37.6% vs. 16.4%; P = 0.000). In six patients elective surgery was indicated immediately after recovery from an episode of CAD.
Some studies have shown relations between BMI and an increased risk of AD [13], recurrent diverticulitis, and CAD [14]. Similarly, some authors have related smoking tobacco to the rate of perforations and postoperative recurrent attacks of AD [15]. Although these factors were not actively considered when proposing elective surgery in our study, related relation was found between tobacco consumption and an elective procedure. Our present trend is towards an individualized selection of patients for elective surgery after a first episode of AD that had been managed conservatively.
Emergent surgery after conservative management
This study provides natural history data from a cohort of patients with AD initially managed without surgery. Thirteen of those 267 patients (4.8%) needed a further emergency operation. The presence of CRF and the type of the first episode of AD were related to the need for urgent surgery in the univariate analysis. Only a first episode of CAD was a risk factor for the need for emergent surgery in the multivariate analysis.
The data on recurrent attacks and the need for emergent surgery are controversial. Anaya and Flum [16] concluded that the risk of emergency surgery increases with increasing number of recurrent attacks. Nevertheless, Ritz et al. [17] found that the risk of free perforation decreased with increasing number of previous episodes of AD. They reported a risk of 5.5% for a colectomy or a colostomy in patients with recurrent AD. Data on recurrences should be observed with caution because some episodes can be managed by a general practitioner or by patient himself without hospital admission. In our experience, the presence of recurrent attacks has not been related to a significant risk of emergent surgery.
The relation between CRF and the need for acute surgery has been described previously. Klarenbeek et al. [18] found that CRF was a risk factor for perforation in 88 patients with recurrent AD. In our study, patients with CRF initially managed without surgery had an increased risk of emergency surgery, but that significance was not maintained in the multivariate analysis.
Although nonoperative management has been suggested after an episode of CAD [19], an elective colon resection has been advised after an episode of CAD. In our experience, 15.9% of the patients diagnosed as having CAD and managed without elective surgery needed an emergent surgical procedure, and this rate of emergency surgery was 5.5 times higher than that in patients diagnosed as having an episode of UAD, being the only significant risk factor for emergent surgery.
Only 37 of the 139 patients initially diagnosed as having a first episode of CAD (26.6%) did not undergo a surgical procedure. These figures are quite similar to those reported by Dharmarajan et al. [5]. They managed without urgent or elective surgery 49 of 136 patients diagnosed as having CAD. Nevertheless, because 84% of the patients with CAD who are managed conservatively do not need a surgical procedure, we think that conservative management may be indicated in selected cases.
Benefit of elective surgery
Interestingly, elective surgery had no protective effect for stoma creation, surgical morbidity, or death compared to nonoperative management. In fact, a higher rate of stoma formation was found after elective surgery than after emergency surgery because four temporal ileostomies were raised in elective surgery due to poor local conditions at the moment of colorectal anastomosis (7.2% vs. 1.4%, P = 0.028). There were no differences between the subgroups of patients with CAD (15.3% vs. 6.8%, P = 0.458) (Table 2). A similar stoma rate of 13.3% was reported by Dharmarajan et al. [5] in elective surgery after an episode of CAD, although in their report, a colostomy was performed more frequently than an ileostomy.
Limitations
Our study has some obvious limitations. First, it is a retrospective study, and the selection for elective surgery, based in more recent reports, has been changing during the period of the study. Second, analysis of recurrences might be difficult because some episodes have been managed by a general practitioner or the patient himself. Moreover, the differentiation between recurrent attacks and persistent symptoms may sometimes be difficult. However, this study is useful because it provides information about how patients progress and the rate of emergency surgery after conservative management of AD.
In conclusion, this study confirms that nonoperative management of AD is safe, even after an episode of CAD, because the majority of patients will not need an emergent procedure in a subsequent attack of AD. There are not differences in the morbidity, mortality, and stoma rates between patients treated with nonoperative management and patients treated with elective surgery. A first episode of CAD is the only risk factor for emergency surgery in patients managed in a conservative form, and an elective colectomy must be considered in these patients. Further investigations focusing on patients with CAD are needed to identify ways to select patients capable of being managed conservatively.
Notes
No potential conflict of interest relevant to this article was reported.