Application of Advancement Flap After Loose Seton Placement: A Modified Two-Stage Surgical Repair of a Transsphincteric Anal Fistula
Article information
Abstract
Purpose
A number of techniques have been described for the treatment of a transsphincteric anal fistula. In this report, we aimed to introduce a relatively new two-stage technique, application of advancement flap after loose seton placement, to present its technical aspects and to document our results.
Methods
Included in this retrospective study were 13 patients (10 males, 3 females) with a mean age of 42 years who underwent a two-stage seton and advancement flap surgery for transsphincteric anal fistula between June 2008 and June 2013. In the first stage, a loose seton was placed in the fistula tract, and in the second stage, which was performed three months later, the internal and external orifices were closed with advancement flaps.
Results
All the patients were discharged on the first postoperative day. The mean follow-up period was 34 months. Only one patient reported anal rigidity and intermittent pain, which was eventually resolved with conservative measures. The mean postoperative Wexner incontinence score was 1. No recurrence or complications were observed, and no further surgical intervention was required during follow-up.
Conclusion
The two-stage seton and advancement flap technique is very efficient and seems to be a good alternative for the treatment of a transsphincteric anal fistula.
INTRODUCTION
Perianal fistula is a very common disease seen in the general population, with a rate of 5.6-12.3/100.000 [1, 2, 3]. According to the cryptoglandular hypothesis, this disease arises from an infectious process of the intersphincteric glands [1, 3]. Generally, fistulectomy is an adequate surgical procedure for the treatment of a simple or low transsphincteric fistula. In the presence of a complicated transsphincteric or suprasphincteric fistula, application of advancement flaps, an anal plug, fibrin glue, ligation of the intersphincteric fistula tract (LIFT), radiofrequency ablation, a loose seton, etc. are among the preferred treatment options [4]. The main objective in all these procedures is the treatment of the disease and the prevention of recurrences and anal incontinence. The cutting seton technique, which has been widely used for years, is associated with a high rate of incontinence. Isbister and Al Sanea [5] reported flatus incontinence, semiformed, and formed fecal incontinence rates after surgery of 36%, 8.5%, and 2.3%, respectively. In another study, the overall postoperative complication rate was reported to be 63%, with a recurrence rate of 6% [6]. Because of the high incontinence and recurrence rates seen after the cutting seton technique, the loose seton technique has become the preferred surgical procedure. Because the fistulous tract is kept open in the loose seton technique, local infection can be controlled more readily and formation of a more complicated fistula can be prevented. In addition, the anal sphincter function can be better preserved. The purpose of this study is to introduce a relatively new technique, application of an advancement after loose seton placement and present our initial results in the treatment of transsphincteric fistula.
METHODS
Between June 2006 and June 2013, 54 patients with the diagnosis of a perianal fistula underwent surgery in our general surgery clinics in Kozyatagi Acibadem Hospital and Istanbul University Cerrahpasa Medical Faculty. The procedures used the cutting seton technique in the 14 patients with an intersphincteric fistula, a fistulotomy in the 27 patients with a simple fistula, and a two-stage loose seton technique and advancement flap in the 13 patients with a transsphincteric fistula. Patients with anal fistula due to Crohn's disease were excluded from the study.
Of the 13 patients who underwent the two-stage loose seton and advancement flap technique, 10 were male patients and 3 were female, with a mean age of 42 years (range, 29-59 years). All patients were informed about the procedure, and informed consent was obtained from each patient. The patients' medical records were prospectively entered into a database, and the data were retrospectively reviewed. In all these patients, only one external orifice of the fistula tract was found, and it was located posterolaterally on only one side of the gluteal region. The internal orifice was localized with pelvic magnetic resonance imaging (MRI) before surgery; then, the two-stage procedure was performed. In the first stage, a loose seton was placed in the fistula tract, and in the second stage, which was performed three months after the first stage, the internal and the external orifices were closed with advancement flaps.
The operation was performed under general anesthesia with the patient in a lithotomy position, and antibiotic prophylaxis was given. In the first stage of the operation, methylene-blue dye was injected from the external orifice of the fistula tract in order to identify the internal orifice; then, a probe was used to trace the tract. Following this, a fistulectomy was done by excising the tract in the gluteal region up to point where the external anal sphincter was located, sparing the sphincter. A loose seton technique was performed with an 8-Fr CH Nelaton silastic tube, encircling both the external and the internal anal sphincters (Fig. 1). One end of the silastic tube was introduced into the other end, and the two ends were tied to each other in order to prevent skin irritation during the postoperative period (Fig. 2). This modification in the seton placement also enabled the seton to move freely by 360° within the tract.
Three months after the seton placement, the patient was readmitted to the hospital for the second stage of the procedure. During the second stage, the previously placed seton was removed, and in order to close the internal and the external orifices of the fistula tract, respectively, a mucosal advancement flap procedure and a house flap (modified V-Y advancement flap) procedure were performed. The two free ends of the flaps were connected to each other at the dentate line with absorbable 3/0 intermittent Vicryl sutures (Figs. 3, 4).
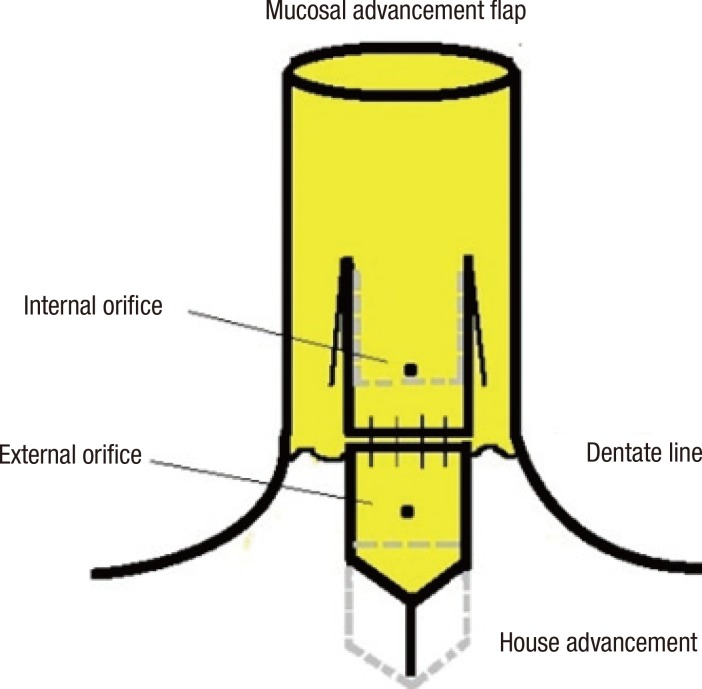
Schematic illustration of the anatomy of the anal canal after the mucosal and the V-Y advancement flap procedures.
During the postoperative period, antibiotic prophylaxis was continued, and pain control was provided by using nonsteroidal anti-inflammatory agents as required. On discharge from the hospital, patients were advised to take a sitz-bath once a day for a week after bowel movements. During follow-up, patients were examined in the clinic in the first, second and fourth postoperative week. After the clinical follow-up, for all the patients, we completed a telephone questionnaire based on the Wexner incontinence scale.
RESULTS
All the patients were discharged on the first postoperative day. The mean follow-up period was 34 months (range, 6-60 months). No complications, including local sepsis, hemorrhage, ectropion, and intractable pain, were noted during the peri- and the postoperative follow-up periods. Of the 13 patients, only one patient reported anal rigidity and intermittent pain during bowel movements, and these symptoms were gradually resolved with conservative measures. The postoperative mean Wexner incontinence score was 1. The success rate regarding anal continence was 100%. No recurrence was observed, and no further surgical intervention was required during follow-up.
DISCUSSION
A perianal fistula is one of the problematic diseases in surgery. Although a number of surgical techniques have been proposed to treat this condition, there is still no single ideal technique for the treatment of this disease. Recently, the LIFT has become a popular procedure [7, 8]; however, the postoperative results after this procedure have not been convincing. The success rate after the first LIFT procedure has been reported to be 67%, and that after a repeated LIFT has been reported to be 90% [9]. In several studies, the advancement flap technique has been compared with other techniques. The mucosal advancement flap is a technique that can be used by itself in the treatment of the perianal fistula and has a success rate between 0% and 83% [10, 11, 12]. One study recommended that ectropion, which is seen after a mucosal advancement flap, could be prevented by using a mucosal V-Y flap, and the success rate was found to be 83% [12]. In addition to these, the loose seton technique is another option for surgical repair. Eitan et al. [13] reported an incontinence rate of 5% after loose seton placement. In another study, the incontinence rate was reported to be 0%-8%, and only minor complaints were observed in 60% of the patients [4, 9].
There are two important problems in the surgical treatment of an anal fistula, recurrence and incontinence, and these two factors affect the surgical outcome. In their series with 60 patients after a mean follow-up period of 24-months, Galis-Rozen et al. [14] reported a complication, including local sepsis and bleeding, rate of 10%. In this series, fecal incontinence was observed in 4 patients, and the recurrence rate was 47%.
In the literature, the success rate after loose seton placement is between 44%-78% [4, 15]. Success rates, of course, depend on the location of the fistula, and they are reported to be 66% and 88% in the presence of anterior and posterior fistulae, respectively [15]. In the presented series with 13 patients, the fistula tract was found to be located posteriorly. Placement of a loose seton by itself does not seem to be a adequate surgical procedure for the treatment of a transsphincteric fistula, which is a rather complicated entity. Because of this, various modifications have been proposed by different authors. Pinedo et al. [4] in their modified loose seton procedure proposed a technique in which the internal orifice was mobilized away from the dentate line by creating a small incision in the internal anal sphincter. This modification keeps the fistula tract dry, which eventually accelerates the healing process. In another study with a different modified loose seton technique, Subhas et al. [16] showed that the seton that was rotated by 360° around the fistula tract by the patient once a day improved the wound healing process in 75% of the patients. However, 25% of the patients did not tolerate this time-demanding treatment. In addition to the seton technique, one of the most commonly performed procedures is the mucosal advancement flap. When performed after the seton placement, the success rate of the mucosal advancement flap is 67%-93% [10, 17].
When compared with the LIFT procedure after seton placement, application of an advancement flap has been reported to contribute to a higher success rate (93.5% vs. 62.5% ) [18]. Eitan et al. [13] investigated 41 patients who had had a loose seton in place for 3 to 7 months and reported that only one patient had loose stool incontinence, two patients had fecal incontinence, and three patients had mucosal wetting during the late follow-up period. In their series of 11 patients who had undergone a mucosal advancement flap (anoplasty) and internal anal sphincter repair after loose-seton application, Zbar [19] reported that 9 patients experienced successful outcomes.
The time period for the removal of the seton is between 2 and 7 months [9, 13]. In our series of 13 patients, we removed the seton after 3 months when the second stage of the operation was scheduled for the patients who had recovered from perianal sepsis. In the second stage, the mucosal and anocutaneous advancement flaps were simultaneously performed. During follow-up, which included the Wexner-incontinence-scale-based telephone questionnaire, the success rate was found to be 100%.
We believe that a single fistula tract, a posterior location of the tract and addition of a modified technique after the placement of a loose seton were the main factors that contributed to our high success rate. We also believe that, although leaving the external orifice open and thus functional helped spontaneous drainage, simultaneous closure of both the internal and the external orifices and application of a V-Y house flap improved wound healing and eventually prevented recurrences by vitalizing the poorly perfused tissues around the external orifice [20].
Based on our results, the two-stage seton and advancement flap technique is very efficient and seems to be a good alternative for the treatment of a transsphincteric anal fistula. Further comparative studies with larger series should be done in order to support our findings.
Notes
No potential conflict of interest relevant to this article was reported.


