Preoperative Localization of Early Colorectal Cancer or a Malignant Polyp by Using the Patient's Own Blood
Article information
Abstract
Purpose
Preoperative localization is the most important preparation for laparoscopic surgery. Preoperative marking with India ink has widely been used and is considered to be safe and effective. However, India ink can cause significant inflammation, adhesions and bowel obstruction. Therefore, we have used the patient's blood instead of the ink since 2011. In this retrospective study, we wanted to examine the feasibility of preoperative localization by using the patient's blood.
Methods
Twenty-five patients who underwent preoperative localization in which 10 mL of their own venous blood was used as a tattooing agent were included in this study. The characteristics of the patients, the anatomy of the colon cancer, and the efficacy and the side effects of using this procedure were analyzed.
Results
In 23 cases (92%), through the laparoscope, we found perfectly localized bloody smudges in the serosa. However, in 2 cases (8%), we could not find the exact location of the lesion. No patients showed any complications.
Conclusion
Preoperative localization of early colon cancer or a malignant polyp by using patient's blood is feasible, safe and simple. We think that using the patient's blood for localization of a lesion is better than using some other foreign material such as India ink.
INTRODUCTION
Incidences of early colon cancer and malignant polyps are rapidly increasing due to frequent regular health checkups. Minimally-invasive surgery, such as a laparoscopic colectomy, is perfectly indicated for these conditions. However, the locations and extents of tumors that are small or flat or that have removed endoscopically may be difficult to establish at surgery. In laparoscopic colorectal surgery in particular, tumor localization cannot be determined because palpation with the fingers is not possible. Thus, preoperative localization of these tumors is important for laparoscopic surgery. Several types of localization techniques have been used: tattooing with India ink or indocyanine green (ICG), clipping the lesion, and intraoperative colonoscopy. However, an animal study questioned the safety and the efficacy of various dilutions of India ink and ICG [1]. Their use caused mucosal ulceration and mild-to-severe inflammation at sites of both concentrated and diluted injections. Also, other studies reported localized peritonitis [2], inflammatory pseudo-tumors [3], intestinal perforations [4], intestinal infarctions [5], and adhesion ileus [6]. To avoid such problems, since 2011, we have used the patient's blood, instead of a foreign material, for tattooing. The purpose of this study was to establish the feasibility of preoperative localization by using the patient's blood.
METHODS
Since May 2011, in twenty-five cases, we used the patient's blood to localize small sized tumors or malignant polyps in colonoscopic tattooing. After approval from the Institutional Review Board, medical records were reviewed. The characteristics of patients, the anatomy of colon cancer, and the efficacy and the side effects of using this procedure were analyzed retrospectively.
Tattooing was performed 24-48 hours prior to laparoscopic surgery. We used 10 mL of the patient's venous blood as a tattooing agent. The blood was taken about 10 minutes before colonoscopy and was not prepared to prevent coagulation. When the lesion was identified, half of the blood was injected submucosally on the distal side of the lesion (about 2 cm below the border of the lesion). The other half of the blood was injected on the proximal side of the lesion (about 2 cm above the border of the lesion).
RESULTS
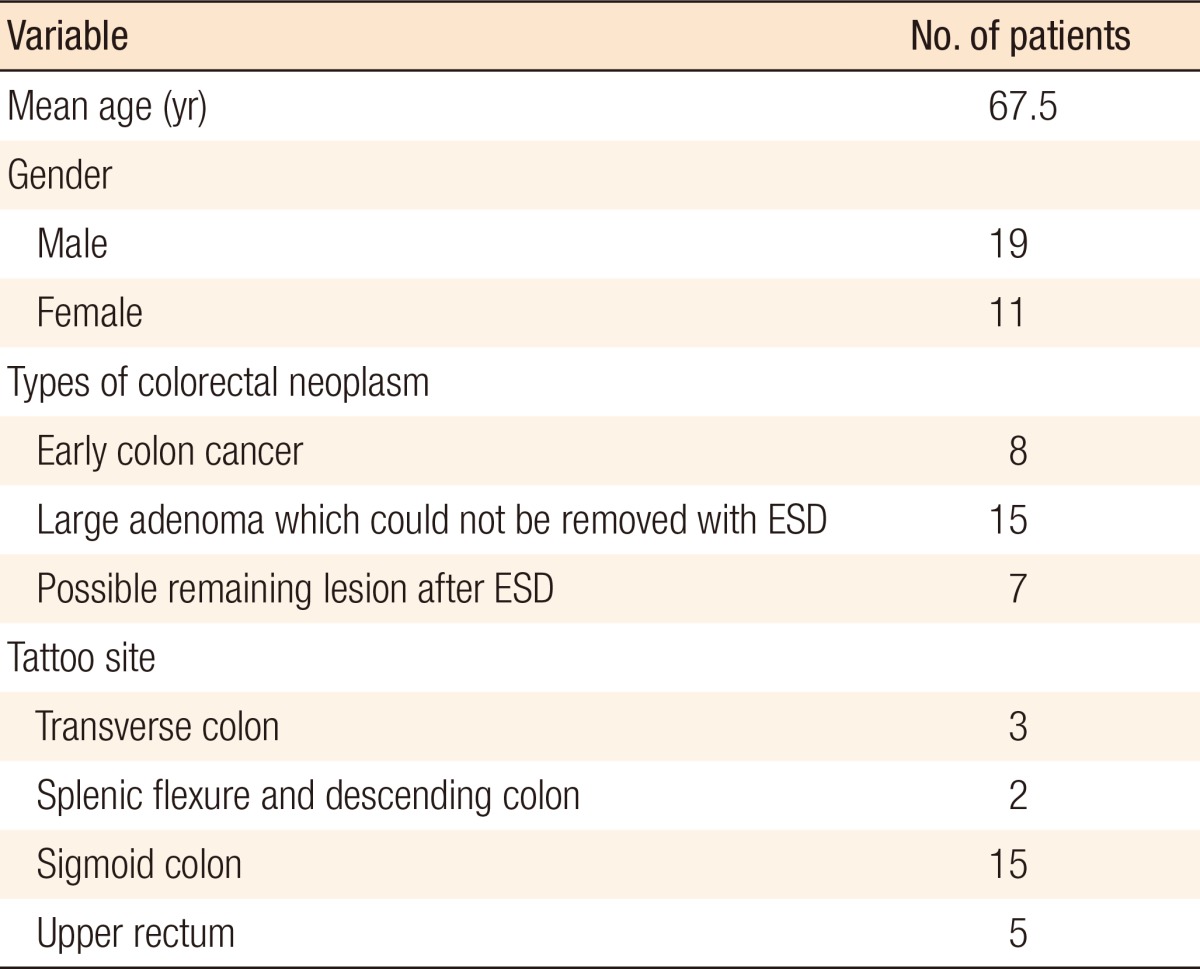
The patients' characteristics are summarized in Table 1. The anatomic distribution of lesions was as follows: transverse colon (n = 3, 12%), splenic flexure and descending colon (n = 2, 8%), sigmoid colon (n = 15, 60%), and upper rectum (n = 5, 20%). In 23 cases (92%), through the laparoscope, we found perfectly localized bloody smudges in the serosa. However, in 2 cases (8%), we could not find the exact location of the lesion. The reasons for failure were an injection that was too deep and an injection that was not deep enough. In the case where the injection was too deep, blood was scattered through the peritoneum adjacent to the affected colon, and in the case where the injection was not deep enough, blood could not penetrate into the serosal layer. There were no complications such as hemorrhage, colonic abscess, or perforation, and none of the patients had clinical symptoms such as fever or abdominal pain after colonoscopy.
DISCUSSION
In this retrospective study, we found that the localization of a small or invisible lesion by using the patient's bloods was an effective, as well as a safe, method. Preoperative localization of colonic lesions is imperative when the lesions are difficult to find at surgery [7]. Localization of a small, serosa-negative lesion is an important issue particularly when the surgery is performed through the laparoscopy because a laparoscopic or laparoscopy-assisted procedure typically compromises tactile feedback. Recently, localization has become more important because the incidence of endoscopic treatment of cancer-bearing polyps is increasing. The polyp site may heal within 2-4 weeks after removal, so the surgeon will unlikely be able to find such a lesion even in open surgery. Several methods of localization have been tried, and their efficacies have been reported [8]. Measurement of the distance from the anus by using colonoscopy has proven to be an inadequate technique for localization in most cases because colonic redundancy may cause looping of the scope, thereby falsely increasing the distance. Cho et al. [9] reported an 88.7% accuracy rate when using colonoscopic distancing alone.
In 1958, Sauntry and Knudtson [10] first reported the technique of tattooing using blue dye at the base of the polyps. Subsequently, Knoernschild [11] reported on a series of 190 patients who underwent endoscopic tattooing. The most commonly used dye is India ink, as first described in 1975 by Ponsky and King [12]. However, endoscopic tattooing with India ink has been associated with complications or side effects. Dye spillage can make the borders vague, and peritoneal ink may closely resemble endometriosis in women [13]. India ink has also been associated with fat necrosis with inflammatory pseudo-tumor formation, colonic abscess, chronic inflammation, and adhesion formation [14, 15]. Also, fluorescence imaging with light-emitting, iodine-activated ICG has been described [16]. Although this technique is reported to be safe and effective, it will add significant cost because the imaging requires a special light and camera.
To avoid the side-effects of using India ink, we designed a fascinating method that uses the patient's blood as a tattooing agent. Because the blood is the patient's, no foreign body or inflammatory reactions should occur. As our results showed, only 5 mL of bloods are required to make a well-demarcated intramural tattoo without any pretreatment preparation in Fig. 1. However, our study has limitations. First, experienced endoscopists performed the procedure. They were fully equipped with the benefits of experience reaped from performing hundreds of cases of colonoscopies. They were able to create well-demarcated tattoos without any complications, such as perforations or misdirections. Secondly, our study involved a very small number of patients. Twenty-five cased are not enough to draw any definite conclusions. We think that further investigations using large numbers of patients will be required if our procedure of using a patient's blood as a tattooing agent is to be accepted as a standard technique for the localization of small colonic cancers.
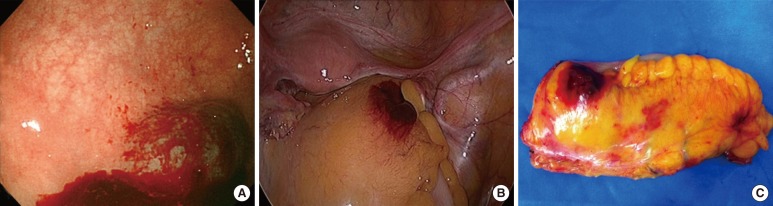
(A) Colonoscopic tattoo with the patient's blood. (B) Intraoperative finding of blood tattoo. (C) Specimen finding of blood tattoo.
In conclusion, tattooing the colonic wall with the patient's blood is a rapid, accurate, and safe technique for localization of small and invisible lesions in the colon. We think that using the patient's blood is better than using any other foreign material in the creation of colonic tattoos. Further investigations regarding the feasibility of our technique and involving larger numbers of patients are warranted.
Notes
No potential conflict of interest relevant to this article was reported.